JCO:李强教授发现基于PRO的主动管理模式能减轻肺癌患者出院后症状负担和并发症
2022-01-15 网络 网络
四川省肿瘤医院李强教授、石丘玲教授团队传来中国最强音!该团队牵头的一项多中心随机对照临床研究(CN-PRO-Lung 2研究)成果,在全球顶尖肿瘤学期刊《Journal of Clinical Onc
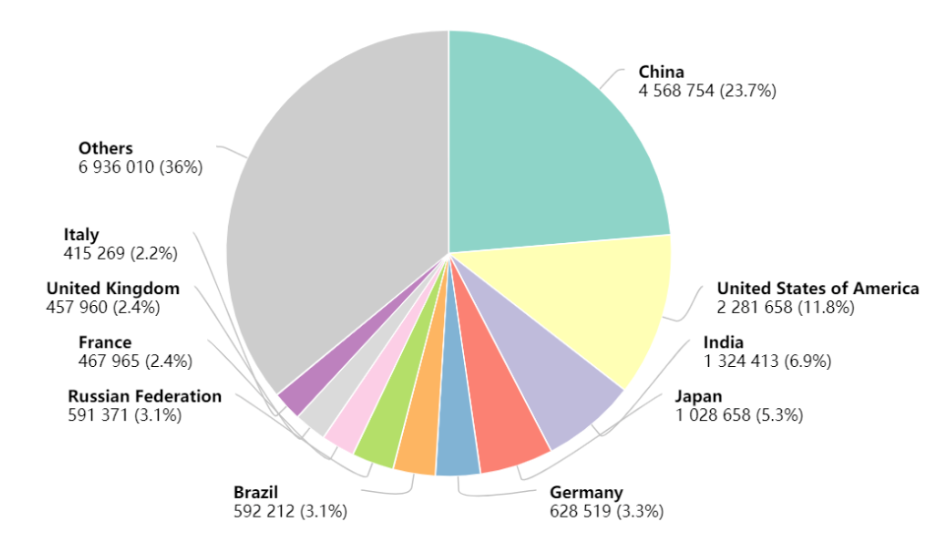
2022年1月8日,四川省肿瘤医院李强教授、石丘玲教授团队传来中国最强音!该团队牵头的一项多中心随机对照临床研究(CN-PRO-Lung 2研究)成果,在全球顶尖肿瘤学期刊《Journal of Clinical Oncology》上发表。 全文链接https://ascopubs.org/doi/abs/10.1200/JCO.21.01344 该研究旨在评估肺癌术后早期,基于患者报告结局(Patient-Reported Outcome, PRO)的症状管理的有效性和可行性。结果显示,基于患者报告结局(PRO)的症状管理模式,可减轻肺癌患者出院后4周内的症状负担和减少并发症。 将手术前,临床诊断为肺癌的患者被1:1随机分配到接受术后基于PRO的症状管理(干预组)或常规护理(对照组)。所有患者在术前、术后每天以及出院后每周两次直到第4周,通过电子PRO系统报告MD安德森症状量表-肺癌子表(MDASI-LC)上的自我症状。在干预组中,预设的5个目标症状(疼痛、乏力、睡眠不安、气短、咳嗽)中的一个超过预警值(≥4分),系统将实时生成警报并发送给医生进行处理。对照组患者仅接受上述PRO症状监测,而无预警和医生主动处理过程。 主要研究结局为患者出院时的症状阈值事件(任何目标症状评分≥4分)的数量,采用PP分析。 研究共纳入患者166例,干预组和对照组各83例。结果显示:出院时,干预组报告的症状阈值事件比对照组少(M[IQR],0[0-2]vs.2[0-3]; P=0.007);在出院后4周,干预组和对照组之间保持了这一差异,(M[IQR],0[0-0]vs.0[0-1];P=0.018)。干预组的并发症发生率明显低于对照组(21.5% vs.40.6%;P=0.019)。医生处理每次预警的中位时间为3分钟。 据悉,该研究为研究者发起的临床研究,由四川省肿瘤医院胸外科中心PRO研究团队负责组织实施。从团队组建、研究设计、项目立项、平台构建、研究实施到成果发表,共历时长达5年之久。 该研究在全球首次验证了基于PRO的主动症状监测-预警-反馈全程管理模式可加速肺癌患者术后康复,且患者满意度高;首次在中国文化背景和医疗体系下,证明了基于PRO的主动管理模式在外科领域有效且有较好的可行性,有利于向临床推广。 研究形成了PRO用于肺癌术后管理的高级别循证医学证据,将为改变患者住院期间“被动式”管理、出院后“散养”状态和解决“看病难”等问题提供新思路,并有望填补国内基于PRO的围手术期全程管理空白。 该成果的发表将促进患者报告结局(PRO)这一新型临床指标在我国恶性肿瘤临床科研及临床实践中的应用,也将奠定四川省肿瘤医院在国内外PRO临床应用研究领域的领先地位。下一步,研究团队将基于《“健康中国2030”规划纲要》,聚焦恶性肿瘤等患者的症状管理模式,开发更多智能化关键技术,在多种疾病和多个地区进行示范推广。 作者简历 供稿:四川省肿瘤医院
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCO#
57
#肺癌患者#
66
#并发#
55
#PRO#
49
#管理模式#
50