Nat Med:PD-L1抑制剂durvalumab联合铂类+培美曲塞治疗既往未治、不能切除的恶性胸膜间皮瘤(MPM)的疗效和安全性:II期临床研究PrE0505
2021-11-16 yd2015 MedSci原创
研究表明,PD-L1抑制剂durvalumab联合铂类+培美曲塞治疗既往未治、不能切除的恶性胸膜间皮瘤(MPM)有显著的临床疗效。
恶性胸膜间皮瘤(MPM)是一种罕见和致命的癌症,治疗选择有限,直到最近批准的免疫检查点抑制剂联合方案。近期,Nature Medicine杂志上发表一项II期临床研究PrE0505 (NCT02899195)的结果,主要是评估抗PD-L1抑制剂durvalumab联合铂类+培美曲塞治疗既往未治、不能切除的恶性胸膜间皮瘤(MPM)的疗效和安全性。

PrE0505是一项II期、单臂、多中心研究,纳入了既往未经治疗、不可切除的MPM患者(NCT02899195)。患者接受durvalumab(固定剂量1,120 mg静脉注射),每3周一次,联合培美曲塞和顺铂,按标准剂量,共6个周期。研究的主要终点是总生存期(OS),定义为从研究登记到因任何原因死亡的时间。
在2017年6月12日至2018年6月21日期间,PrE0505在美国15个学术和社区癌症中心招募了55名患者。中位年龄68岁(范围35-83岁),大多数患者为男性(82%),75%的肿瘤为上皮样组织学。经研究者评估有持续临床获益的患者(n = 20)允许继续。
所有患者均纳入进行疗效分析。在进行分析时,中位随访时间为24.2个月,其中有33例死亡。所有入组患者的中位OS为20.4个月(95%CI: 13.0-28.5, 80% CI: 15.1-27.9),明显长于历史研究对照组的12个月(单侧P = 0.0014),观察到的HR为0.034。评估6个月、12个月和24个月的生存率分别为87.2%、70.4%和44.2%。中位无进展生存期(PFS)为6.7个月(95% CI: 6.1-8.4, 80% CI: 6.3-8.2)。6个月、12个月和24个月时存活和无进展的患者的估计百分比分别为67.3%、18.2%和6.1%。
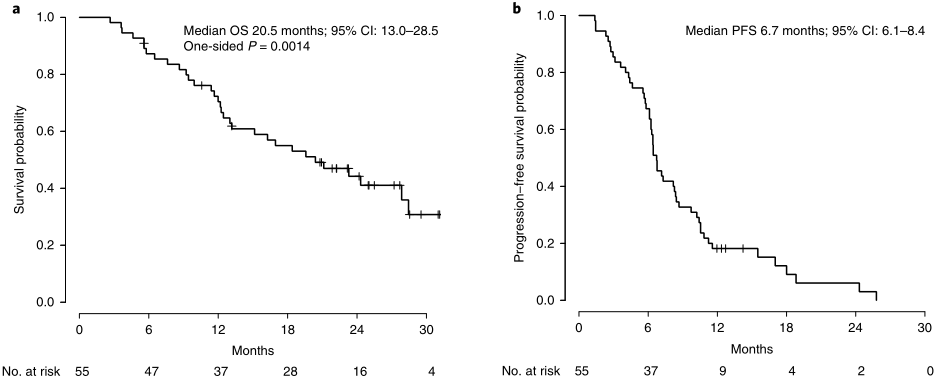
OS和PFS
客观有效率(ORR)为56.4% (95% CI: 42.3-69.7%, 80% CI: 46.8-65.5%)。没有患者出现完全缓解(CR);部分缓解(PR)有31例;20例患者病情稳定。1例患者由于未进行随访疾病评估而无法评估疗效,3例患者出现病情进展(PD)。上皮样肿瘤患者的ORR高于非上皮样肿瘤患者(65.9% vs 28.6%, P = 0.03)。
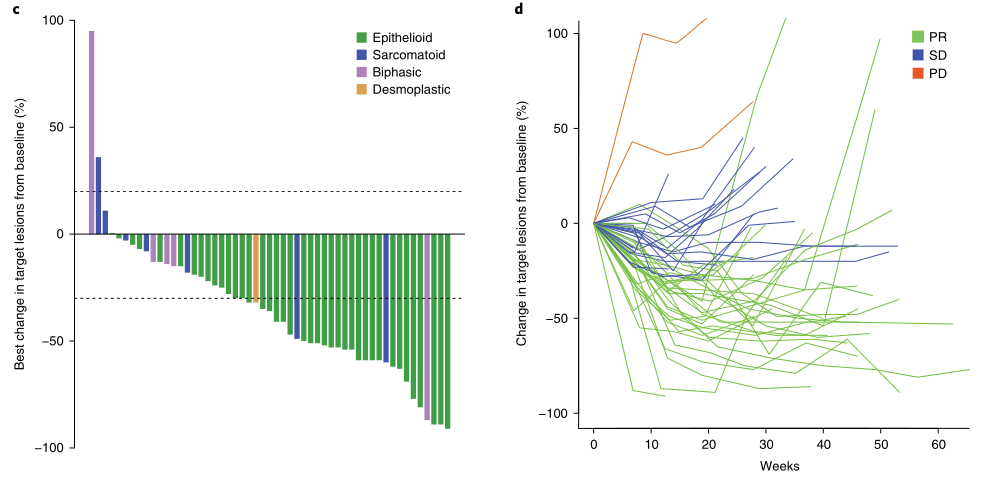
疗效评估
同样,与非上皮样MPM患者相比,上皮样MPM患者的中位OS (24.3个月vs 9.2个月,危险比(HR) = 0.27, 95% CI: 0.13-0.57, P <0.001)和PFS(8.2个月vs 4.9个月,HR = 0.30, 95% CI: 0.16-0.58, P<0.001) 明显较长。

不同病理类型的OS和PFS比较
最常报道的急性治疗不良事件(TEAE)大多是低级别的,包括疲劳(67%)、恶心(56%)和贫血(56%)。3级或更高级别的TEAE发生在65.5%的患者中,包括贫血(20%)、低钠血症(9%)、疲劳(7%)、白细胞减少(5%)、血小板减少(5%)和高血压(5%);所有其他3级或更高的TEAE发生在少于5%的患者中。未观察到5级TEAE。
综上,研究表明,PD-L1抑制剂durvalumab联合铂类+培美曲塞治疗既往未治、不能切除的恶性胸膜间皮瘤(MPM)有显著的临床疗效。
原始出处:
Forde PM, Anagnostou V, Sun Z, et al. Durvalumab with platinum-pemetrexed for unresectable pleural mesothelioma: survival, genomic and immunologic analyses from the phase 2 PrE0505 trial. Nat Med. 2021 Nov 8. doi: 10.1038/s41591-021-01541-0. Epub ahead of print. PMID: 34750557.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
40
#mAb#
44
#抑制剂#
44
#铂#
23
#II期临床研究#
49
#疗效和安全性#
25
#美曲塞#
51
#PD-L1抑制剂#
40
#胸膜#
48
#I期临床#
42