美国临床肿瘤学会(ASCO)年度会议将在2021年6月4日至8日举行,国内外诸多顶级研究成果即将公布。在大会揭幕之前,已有科学人员开始宣布临床研究摘要以及报告的计划。梅斯医学将持续关注并报道学术亮点,分享给各位同道。

ASCO 2021: 摘要概览与展望 5 | 丹娜—法伯癌症研究所ASCO关键研究关注
lenvatinb在不可切除的肝细胞癌患者临床实践中的剂量优化
Lenvatinib已成为不可切除肝细胞癌(u-HCC)患者的一线治疗药物。虽然8毫克或12毫克/天的Lenvatinib是标准起始剂量,但因剂量导致的不良事件发生率很高。在临床实践中,为了应对不良事件的发生,通常使用各种给药方案来减轻毒性。
来自上海复旦大学附属中山医院肝癌研究所研究团队,评估了在中国人群中lenvatinib的两种给药策略的安全性和抗肿瘤活性。结果揭示,通过剂量递增策略或可延长lenvatinib治疗期,与标准疗法相比,具有相当的疗效和更大的耐受性。
在这项研究中,研究人员纳入来自2018年4月至2019年7月间接受lenvatinib进行u-HCC治疗的患者。剂量递增策略如下:开始剂量为4mg/d,每两周递增一次(由于常见的不良事件是在用药后2周内发生),每次递增剂量为4mg。如果没有发生明显的药物相关的不良事件,最终达到8mg或12mg。根据RECIST1.1标准,评估客观缓释率(ORR)和无进展生存期(PFS)。
结果显示,共纳入56名患者,其中剂量递增组为37名患者,标准剂量组为19名患者。剂量递增组的平均体重为64.79公斤,标准剂量组为58.76公斤。根据肝癌分期显示,BCLC C期比例分别为51.4%和63.2%,Child-pugh B期比例分别为16.2%和5.3%。
两组之间的基线人口统计学参数具有可比性(P> 0.05),ORR(32.43%vs 42.1%,P = 0.335),疾病控制率(86.4%vs 84.2%,P = 0.686)和PFS(P = 0.631)均无显著差异。同时,达到全剂量(按体重)的患者比例相似为48.6%和63.2%。标准剂量组的剂量减少率明显高于剂量递增组(36.8%vs 13.5%,P=0.044)。另外,尽管两组之间3/4级不良事件并无显著性差异(P = 0.083),但标准剂量组的患者(36.8%,7/19)比剂量递增组的患者(16.2%,6/37)有更高的G3/4的发生率。
因此,Lenvatinib剂量递增策略可能是患者治疗期的替代疗法。未来需要更多的数据来证实剂量递增策略的长期疗效和安全性。
二线酪氨酸激酶抑制剂(TKIs)与免疫疗法(IO)治疗晚期肝细胞癌的真实疗效和安全性
在过去的四年中,FDA批准了五种药物用于晚期HCC的二线治疗。在美国圣安东尼奥癌症中心,大多数患者都是西班牙裔,且具有不同的肝功能障碍。目前,在TKI和IO的临床注册试验中很少涉及到该人群。
在该项研究中,研究人员对2015年1月至2019年3月对晚期肝细胞癌(HCC)患者进行回顾性分析,这些患者接受了二线治疗,包括IO(即nivolumab)、TKIs(即cabozantinib、regorafenib)或临终关怀/最佳支持性护理(BSC)。
结果显示,在接受一线治疗的患者中,中位年龄为60岁(n=65),患者中75%(n=49)是西班牙裔。58名(89%)患者继续接受二线治疗。hild-Pugh(CP)评分:A 17%,B 55%,C 28%。TKI(n=6)的中位PFS为3.1个月,IO(n=27)为3.3个月,BSC(n=25)为1.3个月。
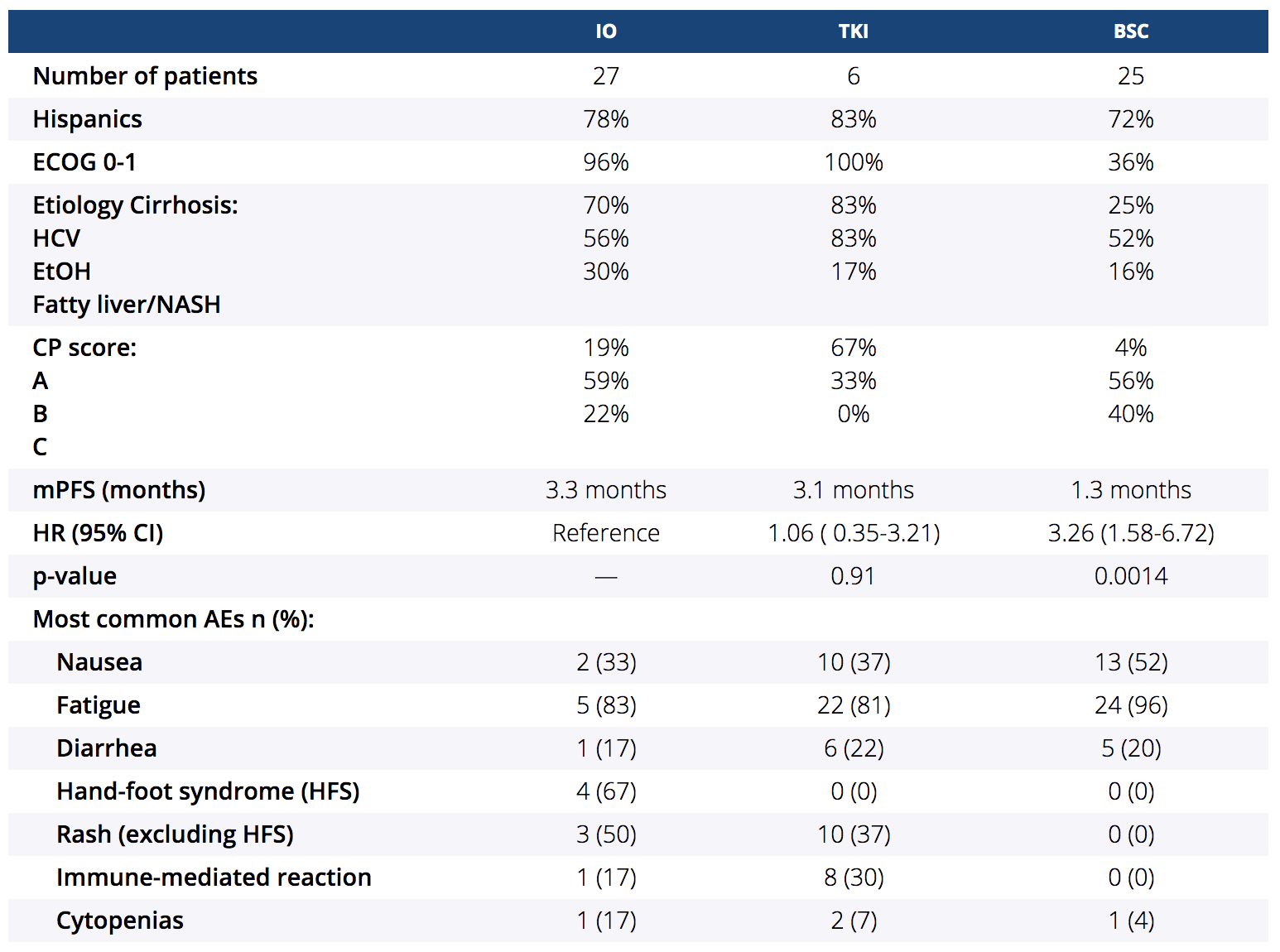
与BSC相比,IO的生存率有所提高(HR=3.26;95%CI:1.58-6.72;P=0.00136)。在比较IO和TKI时没有明显的差异(HR=0.94;95%CI:0.31-2.86;P=0.92),但与BSC相比,TKI有改善PFS的趋势(HR=3.08;95%CI:0.96-9.84;P=0.06)。与IO和BSC相比,TKI组的皮疹(P=0.01)和手足综合征(HFS)(P<0.001)明显增多。所有其他AEs显示组间无明显差异。
综上,在这项以西班牙裔为主的队列研究中,有不同肝功能障碍的患者,包括CP B和C肝硬化,更有可能接受IO或BSC治疗。与BSC相比,两个二线治疗组(IO或TKI)的mPFS都有所增加。与BSC相比,IO和TKI组都是可耐受的,每类药物都有预期毒性。未来,应在不同肝功能障碍的患者中进行更多比较二线药物的前瞻性研究,以了解生存率、耐受性和生活质量。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
48
#肝细胞#
61
#细胞癌#
41
#重磅#
0
#ASCO2021#
79