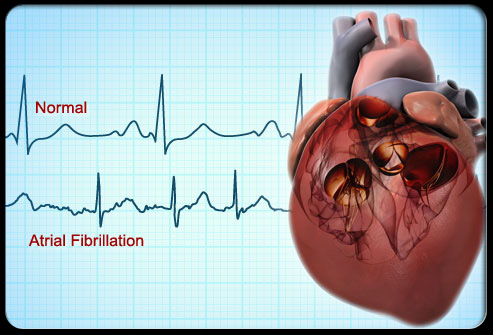
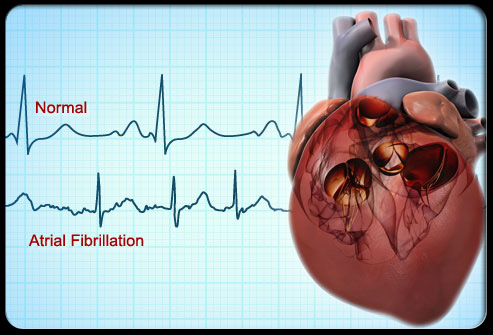
Heart:房颤患者早期不持续性服用达比加群和利伐沙班对临床结局有何影响?
2017-03-13 xing.T MedSci原创
在临床实践中NOAC的非持续服药的发生率较高,达比加群和利伐沙班用药后6个月,大约有三分之一的患者不再持续服药。利伐沙班或达比加群的非持久性服药与较差的卒中/ TIA /死亡等临床预后显著相关。
达比加群和利伐沙班是新型口服抗凝药(NOACs)已被批准用于房颤患者的卒中预防。虽然NOACs与华法林相比更加方便,然而,它们缺乏监测指标可能导致患者不持续性服药。在临床实践中,NOACs不持续性服药的发生率和相关临床结局可用的信息十分有限。近日,在心脏病领域权威杂志Heart上针对这一问题发表了一篇研究文章。
研究人员使用来自于加拿大安大略在1998年1月至2014年3月期间服用达比加群和利伐沙班的房颤患者的管理数据进行了一项回顾性队列研究。不持续性服药的定义是达比加群和利伐沙班的处方间隙超过14天。研究人员采用多变量Cox比例风险模型来估计卒中、短暂性脑缺血发作(TIA)和不持续性服药相关死亡率的主要复合终点。
该研究的队列包括了15857名服用达比加群(80.7岁±6.7岁)和10119名服用利伐沙班(77岁±7.1岁)的患者,各用药组女性占52%。在6个月时,36.4%的患者不再持久性地服用达比加群,而31.9%的患者不再持久性地服用利伐沙班。在非持续性服药的患者中脑卒中或TIA /死亡明显高于那些持续服药的患者,在达比加群组(风险比为1.76(95%可信区间为1.60-1.94);P<0.0001)或利伐沙班组(风险比为1.89(95%可信区间为1.64-2.19);P<0.0001)。相比于那些持续服药的患者,非持续性服药的患者脑卒中/短暂性脑缺血发作的风险明显升高,在达比加群组(风险比为3.75(95%可信区间为2.59-5.43);P<0.0001)和利伐沙班组(风险比为6.25(95%可信区间为3.37-11.58);P<0.0001)。
由此可见,在临床实践中NOAC的非持续服药的发生率较高,达比加群和利伐沙班用药后6个月,大约有三分之一的患者不再持续服药。利伐沙班或达比加群的非持久性服药与较差的卒中/ TIA /死亡等临床预后显著相关。
原始出处:
Cynthia A Jackevicius,et al. Early non-persistence with dabigatran and rivaroxaban in patients with atrial fibrillation. Heart. 2017. http://dx.doi.org/10.1136/heartjnl-2016-310672
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#临床结局#
28
#持续性#
42
学习分享了,谢谢
52
学习了谢谢分享!
60
#ART#
27
#HEART#
0
#房颤患者#
22
谢谢指点迷津
59