美国肾脏护理(USRC)将在透析门诊对COVID-19患者进行单克隆抗体(Bamlanivimab)治疗
2020-12-30 Allan MedSci原创
美国透析服务的主要提供者美国肾脏护理(USRC)公司为26,000多名肾脏疾病患者提供护理,该公司宣布将为其最近诊断为COVID-19的肾脏疾病患者提供单克隆抗体疗法Bamlanivimab。USRC
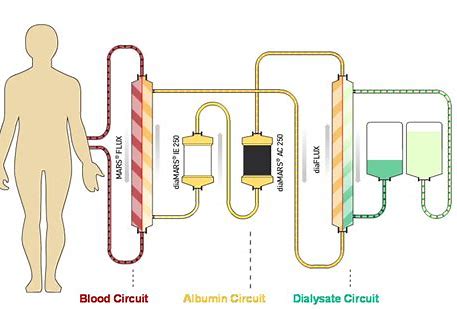
美国透析服务的主要提供者美国肾脏护理(USRC)公司为26,000多名肾脏疾病患者提供护理,该公司宣布将为其最近诊断为COVID-19的肾脏疾病患者提供单克隆抗体疗法Bamlanivimab。USRC借助“Operation Warp Speed”计划和“Project SPEED”计划获得Bamlanivimab,并将在透析门诊中对轻度至中度COVID-19患者使用该药物。
USRC首席医学官Mary Dittrich博士说:“我们的内部数据与来自CMS的数据一致,该数据表明,终末期肾脏疾病患者在罹患COVID-19后,住院率极高。在我们的诊所中,对罹患COVID-19且需要透析的患者进行单克隆抗体治疗可以减少住院治疗和挽救生命”。
Bamlanivimab由Eli Lilly制造,由AmerisourceBergen分销,已获得美国食品药品管理局(FDA)的紧急使用授权(EUA),用于治疗12岁及以上非住院患者的轻至中度COVID-19。
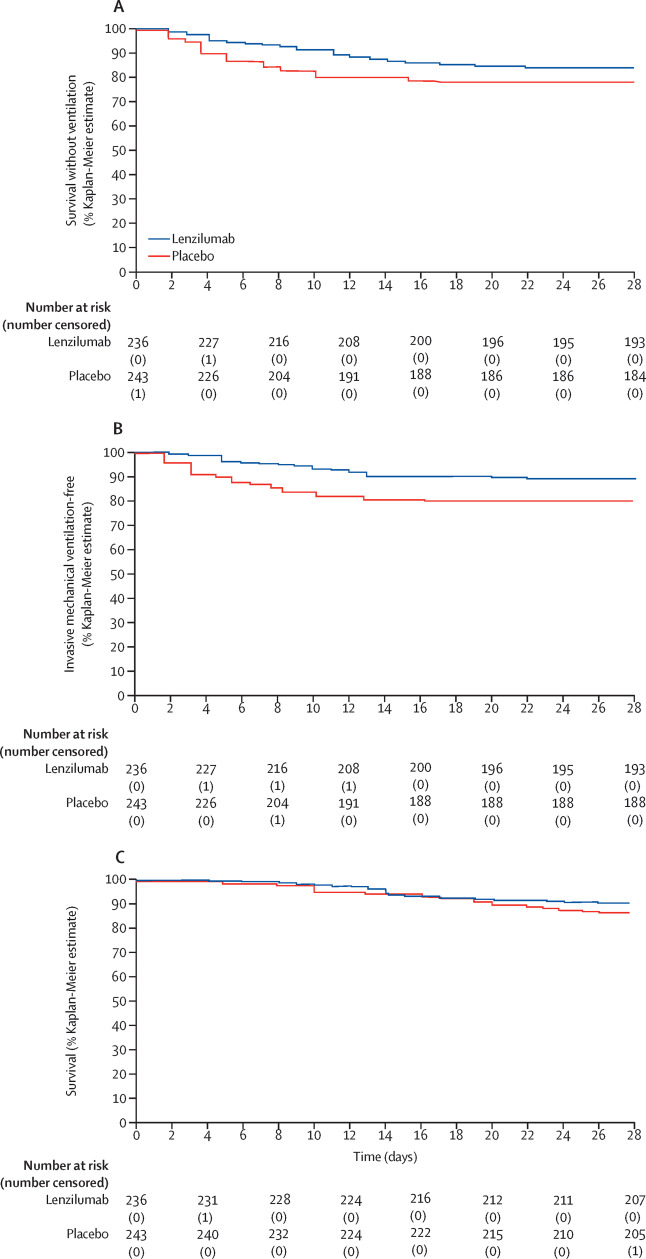
最近在《新英格兰医学杂志》上发表的SARS-CoV-2中和抗体(Bamlanivimab)阻断病毒附着和细胞进入的数据显示,在建议的时限内接受Bamlanivimab治疗的高危患者的住院治疗显著减少。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#SRC#
53
#克隆#
44
#mAb#
46
#NIV#
43
#IVIM#
58
#COVID-19患者#
29
学习
85
学习了
80
最近在《新英格兰医学杂志》上发表的SARS-CoV-2中和抗体(Bamlanivimab)阻断病毒附着和细胞进入的数据显示,在建议的时限内接受Bamlanivimab治疗的高危患者的住院治疗显著减少。
82