ATVB:咀嚼能力与心血管疾病风险生物标志物的关系
2021-06-02 MedSci原创 MedSci原创
与咀嚼能力较差相关的饮食改变以及由此导致的腹部肥胖可能导致IL-6水平升高和NTproBNP水平降低。

近日,心血管领域权威杂志Arteriosclerosis, Thrombosis, and Vascular Biology上发表了一篇研究文章,在当前营养框架下,研究人员假设咀嚼能力差可能是心血管疾病风险升高的早期迹象,该风险是通过全身炎症和心肌细胞应激或损伤的循环标志物来进行评估。
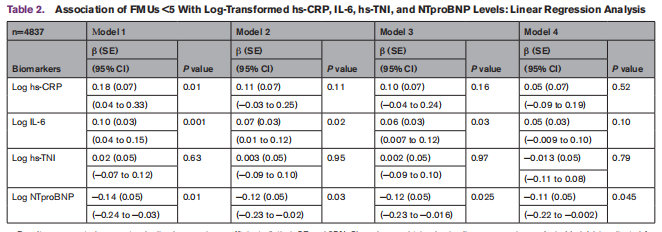
在巴黎前瞻性研究III(一项基于社区的观察性研究)的横断面分析中,4837名50-75岁无心血管疾病史的成年人接受了全口腔临床检查。研究人员采用高灵敏技术测定了受试者血浆中NTproBNP (利钠肽前体n-末端)、hs-CRP(高敏c反应蛋白)、IL-6(白细胞介素-6)、高灵敏肌钙蛋白I (hs-TNI)水平。咀嚼功能较差的定义为功能性咀嚼单位小于5个。
咀嚼能力较差与心血管疾病风险生物标志物的关系
在考虑社会人口统计学因素、心血管疾病危险因素、牙龈炎症和体重指数的线性回归分析中,咀嚼能力较差与较低的NTproBNP水平显著相关(β=−0.11,P=0.045)。在多变量分析中,咀嚼能力较差与较高的IL-6水平之间的显著相关性易受到体重指数的混淆。即使在未经调整的分析中,功能性咀嚼单位和hs-TNI之间也没有相关性。
由此可见,与咀嚼能力较差相关的饮食改变以及由此导致的腹部肥胖可能导致IL-6水平升高和NTproBNP水平降低。
原始出处:
Eirini Chatzopoulou.et al.Poor Masticatory Capacity and Blood Biomarkers of Elevated Cardiovascular Disease Risk in the Community: The Paris Prospective Study III.ATVB.2021.https://www.ahajournals.org/doi/10.1161/ATVBAHA.121.316085
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
40
#TVB#
39
#咀嚼#
40
#疾病风险#
32
#血管疾病#
31
#生物标志#
19
#生物标志#
33