Front Immunol :COVID-19患者的维生素D状况和炎症反应之间的联系
2022-02-20 从医路漫漫 MedSci原创
2020年以来,由新型β型冠状病毒SARS-CoV-2引起的冠状病毒疾病2019 (COVID-19)作为一种大流行出现传播,表现出从无症状到致命的严重急性呼吸综合征(SARS-CoV)的可变表型
背景:2020年以来,由新型β型冠状病毒SARS-CoV-2引起的冠状病毒疾病2019 (COVID-19)作为一种大流行出现传播,表现出从无症状到致命的严重急性呼吸综合征(SARS-CoV-2)的可变表型。研究了多种生物和环境因素,以确定疾病的易感性以及发病率和死亡率的诱发因素。其中,维生素D不足是一个危险因素,并可能成为COVID-19预防或辅助治疗的一个潜在工具。这一建议最初是建立在间接证据的基础上的,即:i)新冠肺炎的季节性火爆恰逢维生素D水平的最低点,ii)维生素D缺乏与肺部感染之间的联系,以及iii)活性激素维生素D(1,25-二羟基维生素D3或骨化三醇)的骨外抗炎作用,这可能有助于抵御所谓的“细胞因子风暴”。
方法:本研究的目的是分析新冠肺炎患者中维生素D状况与炎症标志物生化指标的关系。次要终点是评估25OHD水平与疾病严重程度之间的相关性。从2020年3月至5月,在两个医院对93例新冠肺炎相关肺炎患者进行了评估,这些患者有生化炎症标志物、25-OHD水平、住院期间最低P/F值以及完整的临床资料。
结果:65%的患者出现低维生素D(25-OHD≤20 ng/ml),IL-6[20.8(10.9-45.6)pg/ml比12.9(8.7-21.1)pg/ml,p=0.02],CRP[10.7(4.2-19.2)比5.9(1.6-8.1)mg/dl,p=0.003];D-二聚体为0.53(0.25-0.72)mg/l比0.22(0.17-0.35)mg/l,IL-10为3.7(1.8-6.9)pg/ml比2.3(0.5-5.8)pg/ml,P=0.03],肿瘤坏死因子-α[8.9vs.4.4(1.5-10.6)pg/ml,p=0.01],D-二聚体[0.53(0.25-0.72),vs.0.22(0.17-0.35)mg/l,p=0.03]。即使调整了年龄和性别,25OHD与所有这些指标之间也存在显著的负相关。与其他组相比,严重急性呼吸窘迫综合征患者普遍存在维生素D缺乏(75%vs.68%vs.55%,p<0.001),死亡患者的25-OHD水平较低。
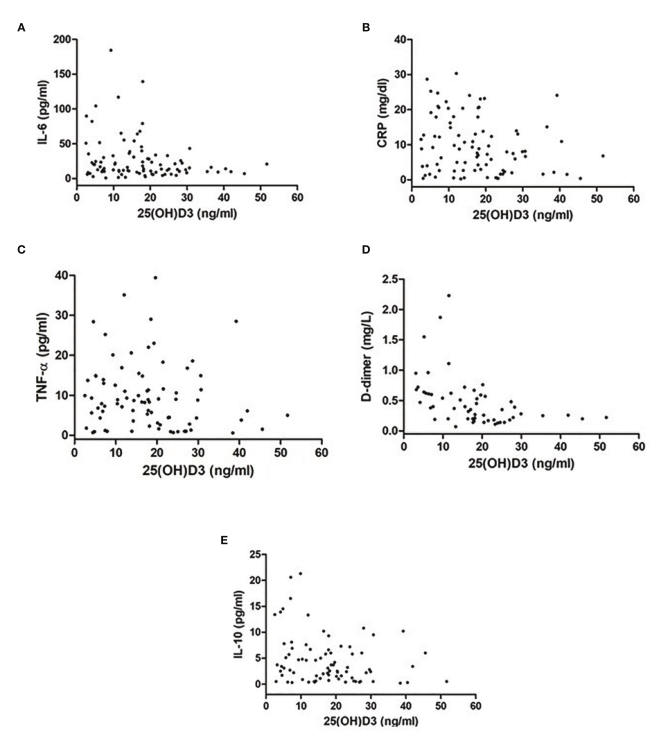
图1 25-OHD水平>20 ng/ml患者与25-OHD水平≤为20 ng/ml患者的炎症标志物[(A)IL-6,(B)CRP,(C)TNF-α,(D)D-二聚体,(E)IL-10]的差异

图2:SARS-CoV-2患者炎症标志物[(A)IL-6,(B)CRP,(C)TNF-α,(D)D-二聚体,(E)IL-10]与25OHD水平的相关性。
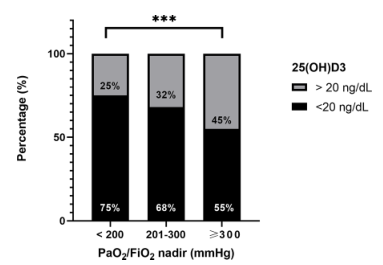
图3 动脉血氧分压/血氧饱和度(PaO2/FiO2)<200、201-300和≤300mmHg的患者中维生素D缺乏患者(25OHD水平≥为20 ng/ml)的比例差异。*p<0.0001。
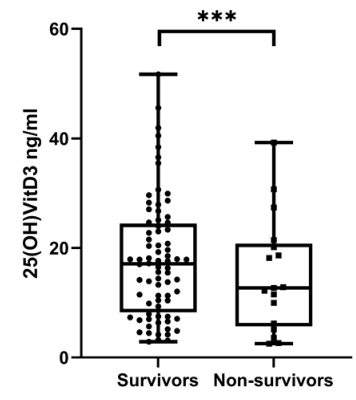
图4 存活和非存活患者25OHD水平差异* * * p < 0.0001。
结论:25-OHD水平与炎症标志物之间的关系提示在这些患者的治疗中需要考虑维生素D的状态。如果维生素D是预后不良的标志,或者是补充维生素D可能带来的有益影响的危险因素,这一点仍然需要阐明。
原文出处:Saponaro F, Franzini M, Okoye C,et al.Is There a Crucial Link Between Vitamin D Status and Inflammatory Response in Patients With COVID-19?Front Immunol 2021;12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









此,建立一个基于患者表型或基因交
44
不错,学习了。
44
学习~~
46
#COVID-19患者#
26
#炎症反应#
40