FDA扩展PARP抑制剂Zejula的适应症,用作晚期卵巢癌的一线维持治疗
2020-05-01 MedSci原创 MedSci原创
与安慰剂相比,Zejula治疗组患者的疾病发展或死亡风险降低了38%。
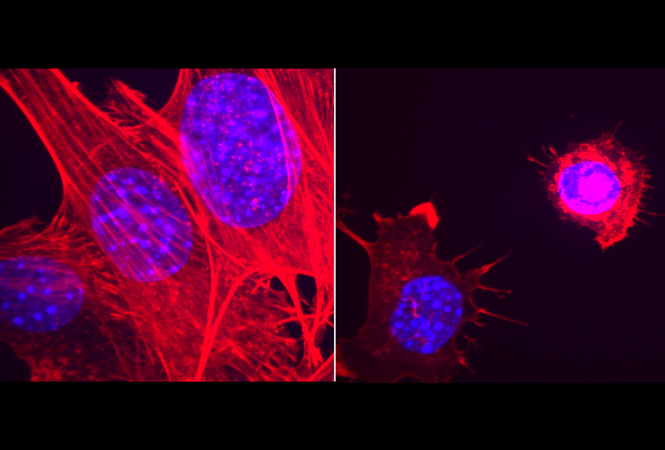
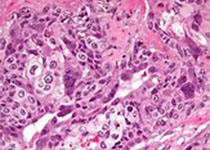
美国食品药品监督管理局(FDA)宣布,已批准葛兰素史克(GlaxoSmithKline)的申请,将PARP抑制剂Zejula(niraparib)单药疗法用作晚期上皮性卵巢癌、输卵管癌或原发性腹膜癌的维持治疗,这些成年人对铂类化疗完全或部分应答,且无论生物标志物状态如何。
GlaxoSmithKline指出,到目前为止,在一线维持治疗中,只有20%的卵巢癌女性(具有BRCA突变的女性)有资格接受PARP抑制剂作为单一疗法的治疗。首席科学官Hal Barron表示,扩大的适应症"意味着更多患有这种毁灭性疾病的女性可以接受Zejula的早期治疗",该药在第一季度的销售额为8100万英镑(1.01亿美元)。
葛兰素史克(GlaxoSmithKline)通过2019年以51亿美元的价格收购 Tesaro获得了这种每日一次的PARP抑制剂,该药物于2017 年首次获准用于对铂类化疗完全或部分应答的复发性上皮性卵巢癌、输卵管或原发性腹膜癌女性的维持治疗。去年10月,该机构批准Zejula用于治疗晚期卵巢癌、输卵管癌或原发性腹膜癌患者,这些患者已经接受了至少三种先前的化疗方案,并且其癌症与同源重组缺陷(HDR)阳性相关。
FDA最新的决定得到了PRIMA III期研究数据的支持,该研究表明,与安慰剂相比,Zejula用作对铂类化疗应答的卵巢癌女性的一线维持疗法,与安慰剂相比,其疾病发展或死亡的风险降低了38%。Zejula组和安慰剂组的PFS中位数分别为13.8个月和8.2个月。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#一线维持治疗#
48
#Zejula#
37
#抑制剂#
40
#适应症#
28
#晚期卵巢癌#
36
#PARP#
28