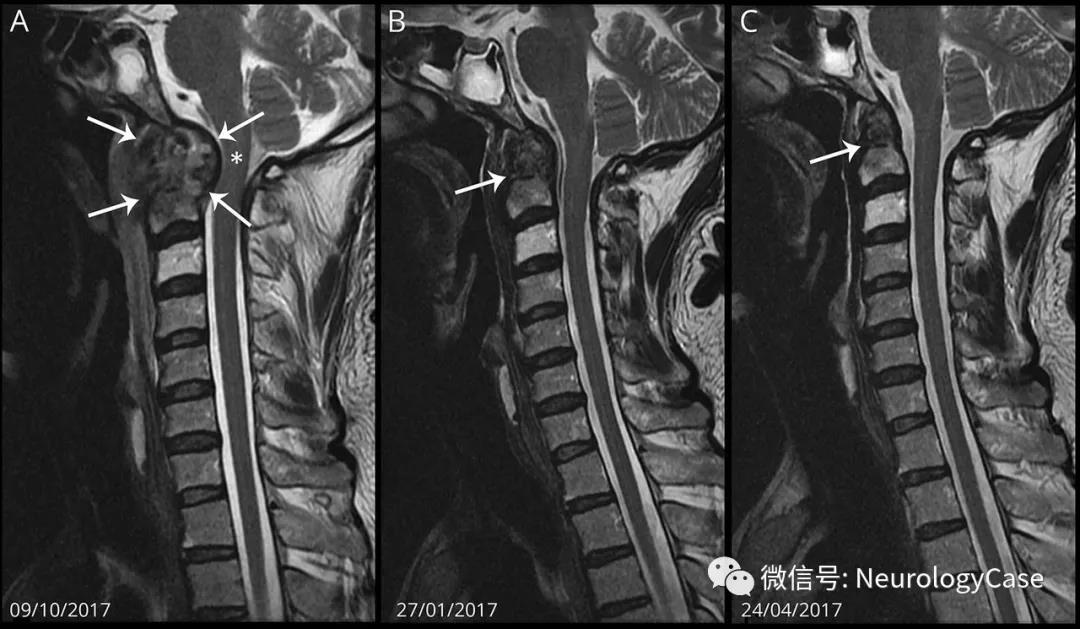
42岁肝硬化男性,MRI可见破坏性的颅颈交界区结核。齿突、轴线椎骨骨质破坏伴不均匀积液(图A,箭),压迫脊髓(图A,*)。开始进行抗结核治疗(ATT),随访复查MRI(图B-C,箭)可见病灶逐渐消退。颅颈交界区结核极为罕见但可危及生命,见于0.3%-1%的结核性脊柱炎患者。几乎所有合并神经功能缺损的患者都需要早期外科干预。在高危手术患者中,等待ATT反应以避免手术-相关的致残和致死是值得的。
(图:A:颅颈交界区矢状位T2WI可见破坏性骨密质改变,齿突周围非均匀积液,导致脊髓明显受压;B-C:抗结核治疗后3个月,积液量和伴随的骨及骨髓变化减少;6个月后病灶完全消退)
原始出处:Philips CA1, Jayarajan TK2. Destructive craniovertebral junction tuberculosis and antituberculosis treatment. Neurology. 2018 Oct 2;91(14):668-669.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Neurol#
31
#结核#
30
#抗结核#
50