Blood:肠道菌群产生的吲哚可通过IFN1限制移植物抗宿主病
2018-09-28 MedSci MedSci原创
中心点:微生物产生或口服的吲哚可限制移植物抗宿主病,且不影响移植抗白血病效应。吲哚通过I型干扰素信号保护和修复粘膜损伤。摘要:异基因骨髓移植(allo-BMT)受体的肠道菌群可调节移植物抗宿主病(GvHD),供体T细胞所引发的全身炎症状态可导致结肠炎(决定GvHD严重程度的关键因素)。肠道菌群色氨酸代谢所产生的吲哚或吲哚衍生物可限制由不同应激源所引发的肠道炎症,因此,研究人员在MHC错配的allo
微生物产生或口服的吲哚可限制移植物抗宿主病,且不影响移植抗白血病效应。
吲哚通过I型干扰素信号保护和修复粘膜损伤。
摘要:
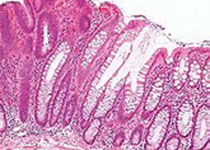
异基因骨髓移植(allo-BMT)受体的肠道菌群可调节移植物抗宿主病(GvHD),供体T细胞所引发的全身炎症状态可导致结肠炎(决定GvHD严重程度的关键因素)。肠道菌群色氨酸代谢所产生的吲哚或吲哚衍生物可限制由不同应激源所引发的肠道炎症,因此,研究人员在MHC错配的allo-BMT小鼠模型中评估吲哚及吲哚衍生物抗GvHD的作用。通过对allo-BMT受体小鼠色氨酸酶阳性或阴性染色的大肠杆菌的定植来评估吲哚的效应,或者通过外源予以吲哚衍生物吲哚-3-羧基醛(ICA)来评估。
ICA治疗可限制肠上皮损伤、减少经上皮的细菌移位,同时减少炎性细胞因子产生、减轻GvHD病理以及降低GVHD死亡率,而且不影响供体T细胞介导的移植物抗白血病(GvL)反应。ICA治疗还可促进受体特异性耐受移植T细胞。转录谱和基因本体分析提示ICA治疗可上调与I型干扰素(IFN1)反应相关的基因,这些基因已被报道可抵抗放射诱导的肠损伤和减轻GvHD病理。因此,在缺乏IFN1信号的小鼠中,ICA在放射暴露后的保护作用被消除。
总而言之,本研究提示肠道菌群所产生的吲哚代谢可通过I型IFNs限制与清髓性放化疗和急性GvHD相关的肠道炎症和损伤,而且不影响抗肿瘤反应,或可为有GvHD风险的BMT患者提供新的治疗选择。
Alyson Swimm, et al. Indoles derived from intestinal microbiota act via type I interferon signaling to limit Graft-versus-Host-Disease. Blood 2018 :blood-2018-03-838193; doi: https://doi.org/10.1182/blood-2018-03-838193
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#植物#
28
学习了
66
#肠道菌#
29
#宿主#
34
#移植物抗宿主病#
30
#IFN#
42
#移植物#
30