Martin Wilkins: 肺动脉高压遗传学 迎来新篇章
2018-08-06 陈小曦 中国循环杂志
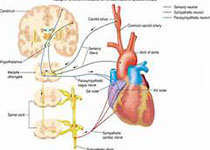
在肺血管病论坛上,英国医学科学院院士、帝国理工学院医学院副院长Martin R. Wilkins 教授指出,目前全球肺动脉高压基因遗传学研究正蓬勃发展,取得了不少研究成果,为寻找新的药物关键作用靶点奠定了基础。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习
75
#新篇章#
53
#动脉高压#
0
#遗传学#
38
#ART#
34
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
49
学习
78