Leuk Lymphoma:阿扎胞苷或可降低老年AML患者不良事件发生率
2017-05-04 梁舒瑶;常路 环球医学
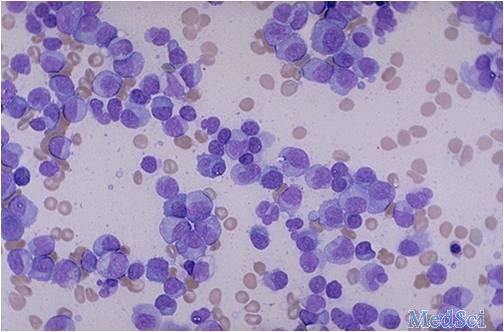
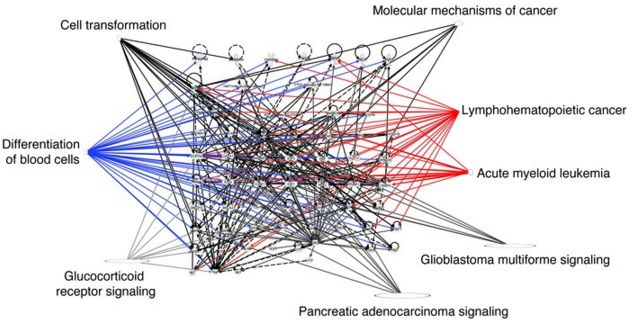
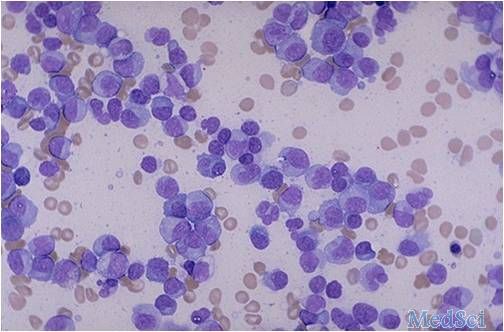
阿扎胞苷是一种新型表观遗传学抗肿瘤药。2017年6月,发表在《Leuk Lymphoma》的一项研究表明,急性髓细胞性白血病老年患者中,与常规治疗方案相比,阿扎胞苷可降低治疗中出现的不良事件及其相关住院的发生率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#lymphoma#
35
#发生率#
32
涨知识,学习了
52
化疗在白血病的治疗中的作用越来越重要。
55
疗效有没有减低呢?
62
学习了,不错
46
还要有更多资料
64
谢谢了,学习
24
学习了,谢谢分享
23
学习了,谢谢分享
26