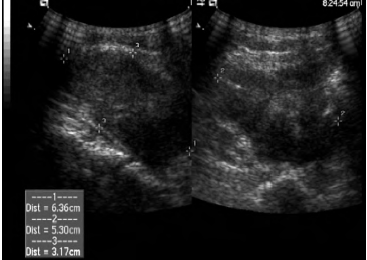
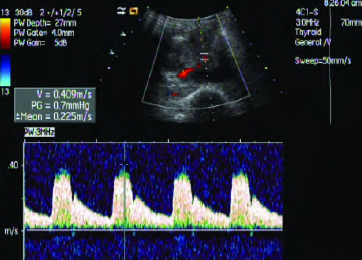
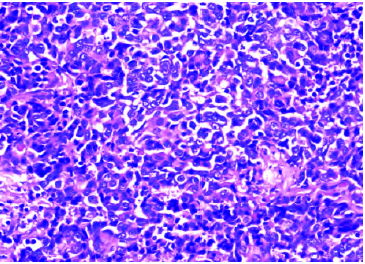
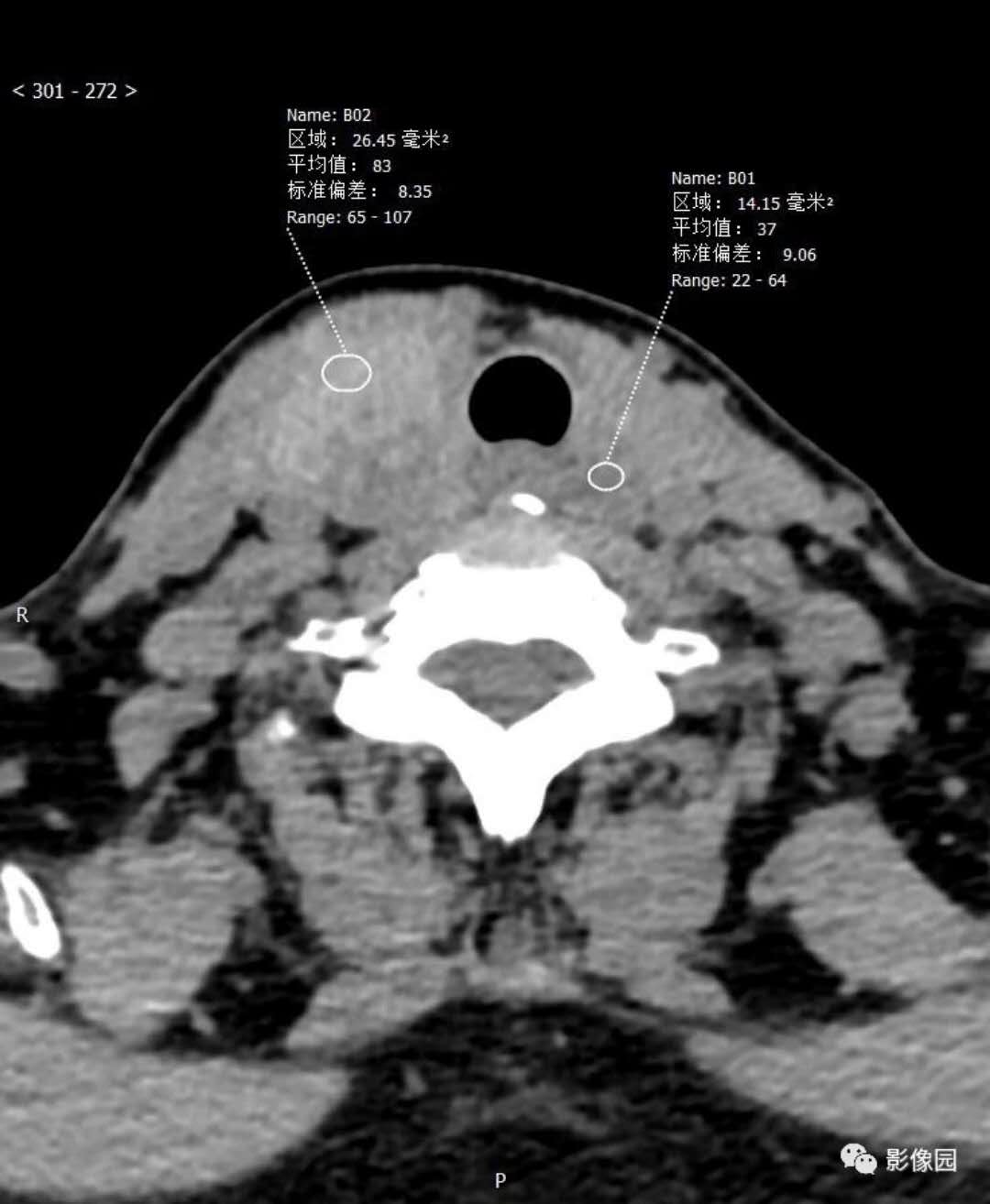
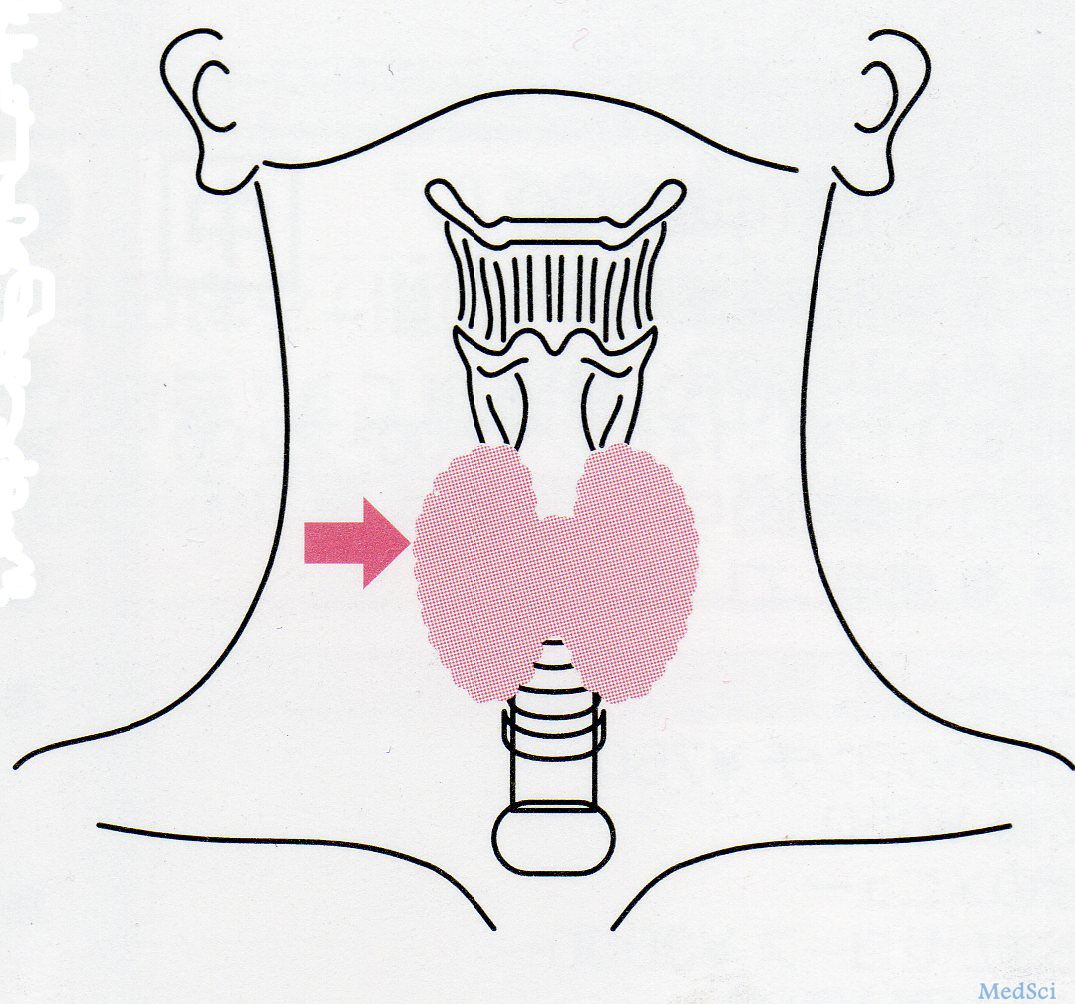
甲状腺呈胸腺样分化癌超声表现1例
2019-01-25 刘捷 章晓锋 临床超声医学杂志
患者男,39岁,因急性支气管炎入院。自诉反复咳嗽10+d,以干咳为主,伴少许白色泡沫痰,无发热、盗汗,无咯血、胸痛及声音嘶哑。体格检查:生命体征稳定,神志清楚,右侧甲状腺呈Ⅲ度肿大;双肺呼吸音稍低,未闻及明显啰音;心率100次/min,律齐,无杂音;腹软,无压痛,肝脾肋下未触及;双下肢无水肿。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胸腺样#
36
#胸腺#
27
#分化癌#
41
#超声表现#
37
讲解很透彻,与实际相结合,
73