Br J Cancer:贝洛替康与拓扑替康治疗复发性卵巢癌的2b期临床研究
2020-10-11 xiaozeng MedSci原创
研究显示,卵巢癌的预后较差,目前确诊的三分之二以上的患者已处于IIIC–IV期,且患者的5年生存率<30%。
研究显示,卵巢癌的预后较差,目前确诊的三分之二以上的患者已处于IIIC–IV期,且患者的5年生存率<30%。
复发性卵巢癌患者根据初次化疗完成后的复发时间分为两类,复发时间>6个月的患者被归类为铂敏感性复发性卵巢癌(PSROC),而≤6个月则为铂耐药性复发性卵巢癌(PRROC)。铂类化疗对于PSROC患者对仍然有效,反应率高达65 %,相比之下,PRROC患者即使使用非铂类药物,但其缓解率仍低于30%。
这项Phase 2b期临床研究旨在比较在复发性卵巢癌中贝洛替康(Belotecan)和拓扑替康(Topotecan)的功效和毒性。
患者治疗策略分类
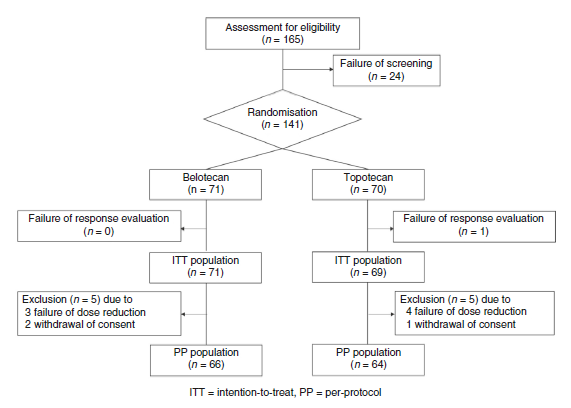
在该临床试验中,PSROC或PRROC患者采取每3周连续五天按1:1的比例接受0.5μmg/m2贝洛替康或1.5μmg/m2拓扑替康给药。临床试验的主要终点为总体缓解率(ORR),次要终点为无进展生存期(PFS),总生存期(OS)和药物毒性。
该研究分别募集到意向性分析(ITT)和遵循研究方案分析(PP)的140例(贝洛替康,n = 71;拓扑替康,n = 69)和130例(贝洛替康,n = 66;拓扑替康,n = 64)患者。
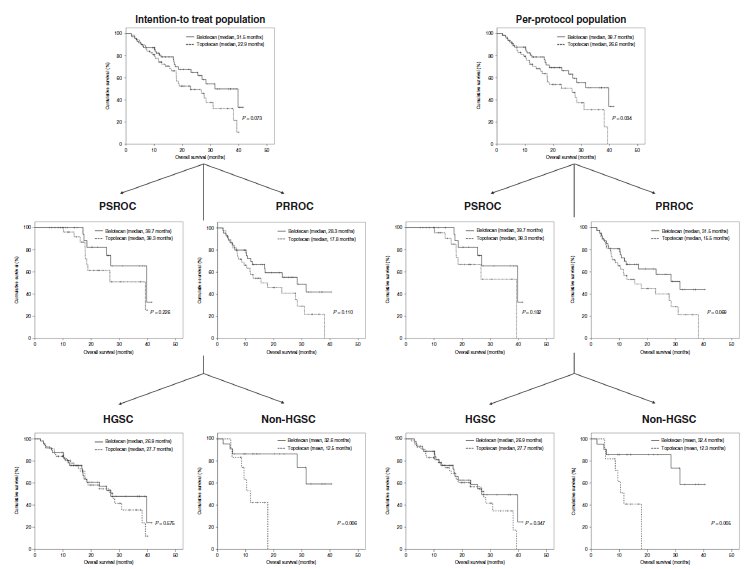
贝洛替康和拓扑替康的总生存期比较
结果显示,在贝洛替康组和拓扑替康组中,患者的总体缓解率无显著差异(ITT,29.6%对26.1%; PP,30.3%对25%)。尽管两组的无进展生存期没有差异,但相比于PP中的拓扑替康组,贝洛替康能够更好的改善患者的总生存期(39.7对26.6个月)。
特别的是,在PRROC和非高级别浆液性癌中,贝洛替康组显示出更长的总生存期。此外,两组的药物毒性结果并无显著差异。
综上,该研究结果显示,就复发性卵巢癌的整体反应而言,贝洛替康的治疗效果不逊于拓扑替康。
原始出处:
Kim, H.S., Park, S., Park, C. et al. A multicentre, randomised, open-label, parallel-group Phase 2b study of belotecan versus topotecan for recurrent ovarian cancer. Br J Cancer (30 September 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#复发性#
28
#2b期临床#
33
#复发性卵巢癌#
30
学习
94
学习
82
学习了
96
#贝洛替康#安全性如何?
135
阅读谢谢分享
96