Lancet:曲妥珠单抗对HER2阳性早期乳腺癌的11年随访结果
2017-03-25 xingxiaowei MedSci原创
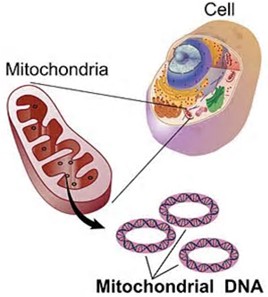
曲妥珠单抗是HER2受体的单克隆抗体,可以显着增加HER2阳性早期乳腺癌患者的总生存期以及无病生存期。但是对于其疗效的长时间的随访数据仍然缺乏。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#随访结果#
21
#曲妥珠#
33
#Lancet#
22
#HER2阳性#
25