JCEM:水果摄入量与糖尿病风险之间的关联
2021-06-03 MedSci原创 MedSci原创
所有水果但不包括果汁在内的健康饮食可能在降低T2DM风险方面发挥着重要作用。
水果,而非果汁,摄入量与2型糖尿病 (T2DM)之间呈负相关。然而,关于水果可能发挥保护性作用的机制仍未明确。

近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在评估摄入的水果类型与1) 葡萄糖耐量和胰岛素敏感性指标以及 2) 随访时发生糖尿病之间的关联。
在澳大利亚糖尿病、肥胖和生活方式研究的参与者中,研究人员通过基线摄入食物频率问卷来评估水果和果汁的摄入量。研究人员在Logistic和线性回归模型中使用受限三次样条评估了水果和果汁摄入量与1)基线空腹血糖、餐后2小时血糖、β细胞功能的HOMA2 (HOMA2-%β)、胰岛素敏感性的HOMA2(HOMA2-%S) 和空腹胰岛素水平之间的关联,以及2)其与随访时(5年和12年)糖尿病之间的相关性。
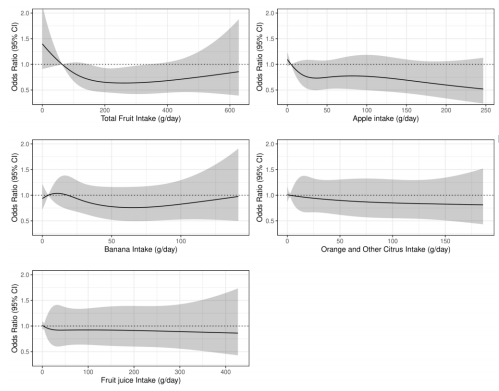
水果、果汁摄入量与糖尿病风险
该研究的7675名澳大利亚参与者(45%为男性)基线时的平均年龄为54±12岁。总水果摄入量与血清胰岛素和HOMA2-%β之间呈负相关,而与基线时的 HOMA2-%S呈正相关。在调整饮食和生活方式混杂因素后,与摄入量最低(四分位数为1)的参与者相比,总水果摄入量中等(四分位数为3)的参与者在5年内患糖尿病的几率降低了36%[OR(95%CI): 0.64(0.44-0.92)],而水果摄入量与12年结局之间的相关性没有统计学意义。
由此可见,所有水果但不包括果汁在内的健康饮食可能在降低T2DM风险方面发挥着重要作用。
原始出处:
Nicola P Bondonno.et al.Associations between fruit intake and risk of diabetes in the AusDiab cohort.JCEM.2021.https://doi.org/10.1210/clinem/dgab335
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#摄入量#
46
#JCE#
41
#JCEM#
34
学习了
54
学习学习
54
谢谢MedSci提供最新的资讯
44