Gastroenterology.:水下内镜下黏膜切除术可提高肠息肉的切除率
2019-08-06 MedSci MedSci原创
UEMR显著增加了10-20mm无蒂结直肠病变的R0切除率
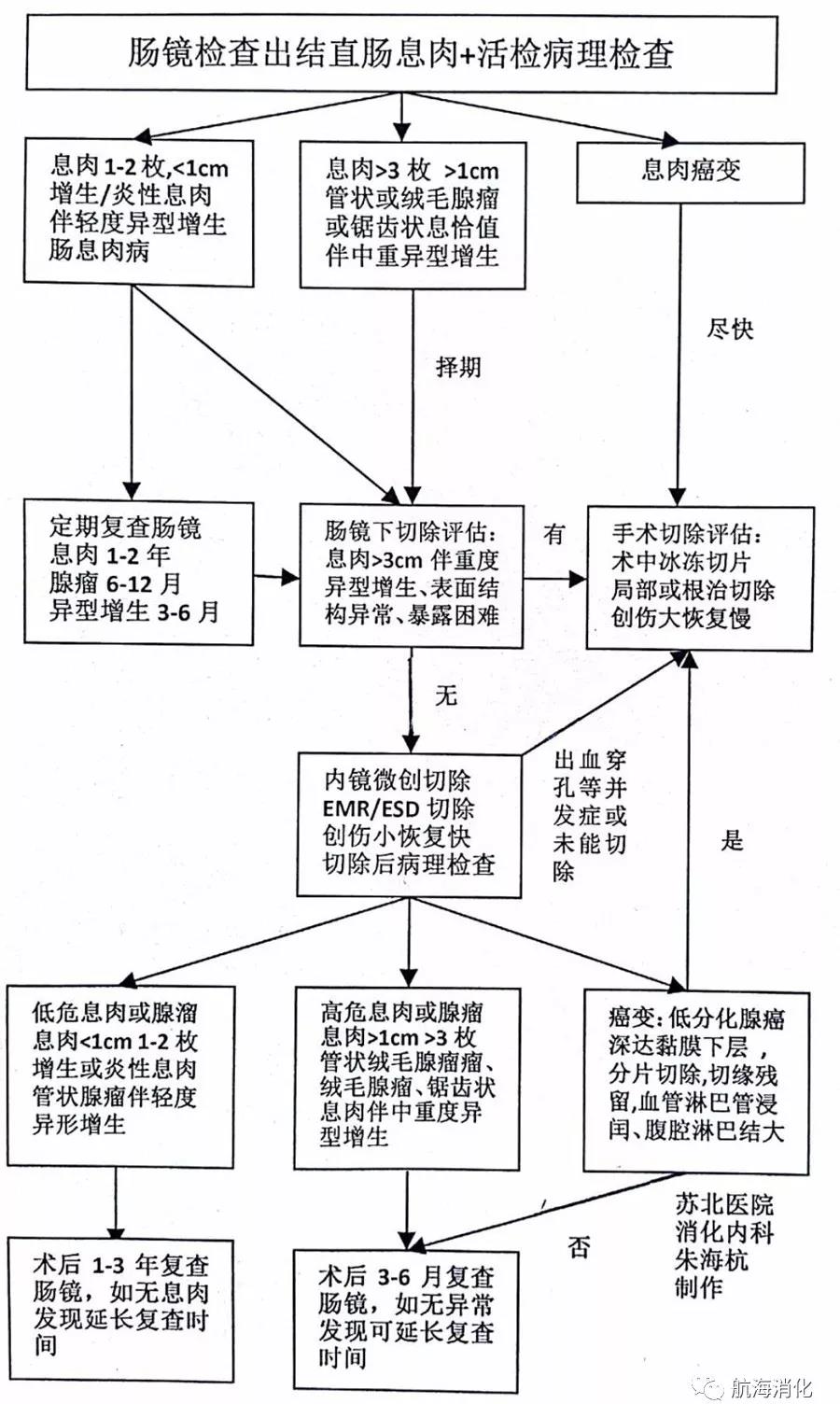
内镜下黏膜切除术(EMR)结合黏膜下注射是切除大肠息肉的一种有效方法,但当息肉直径超过10 mm时,整体切除率降低。局部切除增加局部复发。水下EMR(UEMR)是一种有效的切除无梗结直肠息肉的技术,近日研究人员就EMR对大息肉的切除效果进行了考察。
研究在日本开展。经内镜诊断为中等大小(10~20 mm) 无蒂结直肠病变的患者随机分为接受UEMR或常规EMR(CEMR)。EUEMR手术将整个管腔浸入水中,在不注射生理盐水的情况下切除病变。研究的主要终点是各组间组织学证实为阴性切缘的整块切除(R0)率的差异。
EUEMR组R0切除率为69%,CEMR组为50%。EUEMR组整体切除率为89%,CEMR组为75% (P=0.007)。组间中位手术时间(165 vs 175秒)和不良事件患者比例(UEMR组为2.8%,CEMR组为2.0%)无显著性差异(P>0.05)。
研究认为,UEMR显著增加了10-20mm无蒂结直肠病变的R0切除率。
原始出处:
Takeshi Yamashina et al. Comparison of Underwater vs Conventional Endoscopic Mucosal Resection of Intermediate-Size Colorectal Polyp. Gastroenterology. August 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#GAS#
21
#Gastroenterol#
25
#AST#
17
#切除术#
18
#内镜#
24
#Gastroenterology#
21
#黏膜#
0