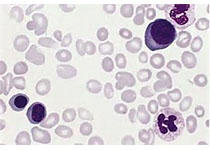
Blood:达雷木单抗联合卡非佐米/地塞米松(Dkd)为来那度胺难治性多发性骨髓瘤患者带来新的希望
2019-05-22 QQ MedSci原创
复发性或难治性多发性骨髓瘤(RRMM)患者的治疗方案有限,存活预后较差。当下,越来越多的选用以来那度胺为基础的疗法作为MM的一线疗法,因此,需要针对来那度胺难治性患者开发新的有效疗法。
中心点:
无论既往是否采用过来那度胺治疗,达雷木单抗(Daratumumab)联合卡非佐米(carfilzomib)/地塞米松可诱导多发性骨髓瘤患者获得深层次、持久的缓解。
摘要:
复发性或难治性多发性骨髓瘤(RRMM)患者的治疗方案有限,存活预后较差。当下,越来越多的选用以来那度胺为基础的疗法作为MM的一线疗法,因此,需要针对来那度胺难治性患者开发新的有效疗法。
研究人员开展一个1b期研究,招募了85位既往治疗过1-3次(包括硼替佐米和免疫调节剂)的来那度胺难治性的MM患者,评估达雷木单抗联合卡非佐米和地塞米松(Dkd)用于该患者的疗效和安全性。
所有患者接受卡非佐米(初始剂量20mg/m2,随后递增至70mg/m2,每疗程的第1、8和15天给药)和地塞米松(40mg/周)治疗。达雷木单抗的给药方式:10位患者单次注射(16mg/kg,第1疗程的第一天给药),另75位患者予以分次注射(8mg/kg,第1疗程的第一、二天给药)。随后给药方式相同。患者既往治疗疗程中位值为2(1-4);60%为来那度胺难治性。
最常见的3/4级需紧急治疗的副反应有血小板减少(31%)、淋巴细胞减少(24%)、贫血(21%)和中性粒细胞减少(21%)。首剂单次注射和分次注射组分别有60%和43%的患者发生输液相关反应。总体缓解率达84%(79%为来那度胺难治性)。随访期间未达到中位无进展存活期(PFS);所有患者和来那度胺难治性患者的12个月PFS率分别为74%和65%。
综上所述,D-kd疗法用于多发性骨髓瘤患者,包括对来那度胺难治性的患者,耐受性良好,副反应率低,可诱导深度缓解和较高的PFS率。
原始出处:
Ajai Chari, et al. Daratumumab Plus Carfilzomib and Dexamethasone in Patients With Relapsed or Refractory Multiple Myeloma. Blood 2019 :blood.2019000722; doi: https://doi.org/10.1182/blood.2019000722
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#多发性#
25
#达雷木单抗#
41
#难治性#
33
#DKD#
48