NEJM:无ST段抬高的院外心脏骤停患者该何时血管造影?
2021-12-30 MedSci原创 MedSci原创
在没有ST段抬高的院外心脏骤停复苏的患者中,就30天全因死亡风险而言,即刻进行血管造影的策略与延迟或选择性策略相比并没有任何益处。
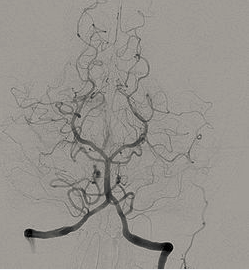
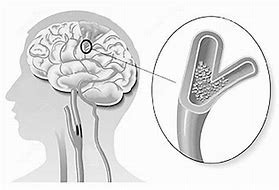
心肌梗塞是院外心脏骤停的常见原因。然而,在心电图上没有ST段抬高证据的复苏患者中,早期冠状动脉造影和血运重建的益处尚未明确。
近日,顶级医学期刊NEJM上发表了一篇研究文章,在这项多中心试验中,研究人员随机分配了554名可能是冠状动脉起源的院外心脏骤停成功复苏的患者,分别接受即刻冠状动脉造影(即刻血管造影组)或延迟或选择性血管造影。
所有患者在复苏后心电图上均未发现ST段抬高的证据。该研究的主要终点是30天时的任何原因死亡,该研究的次要终点包括30天时全因死亡或严重神经功能缺损的复合结局。
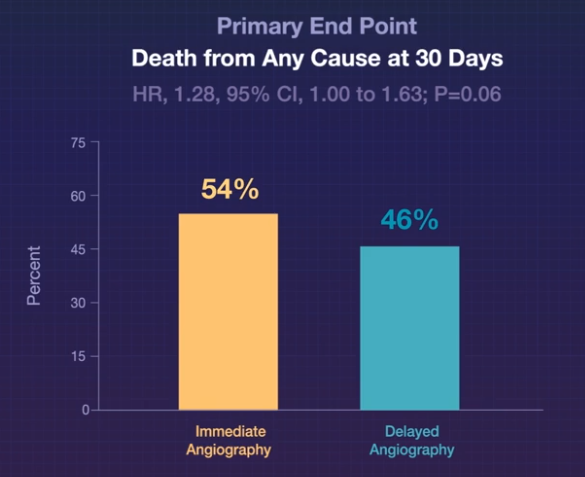
该研究主要分析纳入了554名患者中的530名(95.7%)受试者。在30天时,即刻血管造影组265名患者中的143名(54.0%)患者和延迟血管造影组265名患者中的122名(46.0%)患者死亡(风险比为1.28;95%置信区间[CI]为1.00到1.63;P=0.06)。与延迟血管造影组(248名患者中的138名[55.6%]患者)相比,即刻血管造影组(255名患者中的164名[64.3%]患者)更常发生死亡或严重神经功能缺损的复合事件。相对风险为1.16(95%CI为1.00到1.34)。两组的峰值肌钙蛋白释放值和中度或重度出血、卒中和肾脏替代治疗的发生率相似。
由此可见,在没有ST段抬高的院外心脏骤停复苏的患者中,就30天全因死亡风险而言,即刻进行血管造影的策略与延迟或选择性策略相比并没有任何益处。
原始出处:
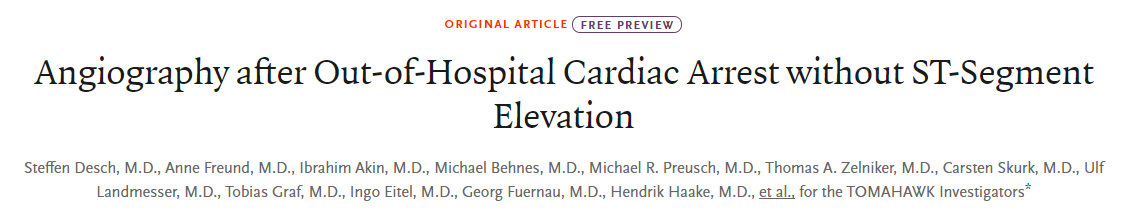
Steffen Desch,et al.Angiography after Out-of-Hospital Cardiac Arrest without ST-Segment Elevation.NEJM.2021.https://www.nejm.org/doi/full/10.1056/NEJMoa2101909
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#院外心脏骤停#
46
#ST段抬高#
44
#造影#
43
#ST段#
57