Stroke:淀粉样血管病与执行功能障碍和轻度认知功能障碍相关
2016-06-29 phylis 译 MedSci原创
背景:尸检研究表明,脑淀粉样血管病(CAA)与认知功能障碍和痴呆发生风险相关。研究者分析前瞻性队列研究中CAA患者的神经心理学测验的数据,识别认知障碍的发病率及脑磁共振成像特点和载脂蛋白E基因相关性。方法:数据来自34民航局分析,16阿尔茨海默病,69轻度认知障碍,27的缺血性中风的参与者。神经心理测试结果表示为Z分数的测试手册提供的规范性数据,然后分为域的内存,执行功能和处理速度。结果:CAA受
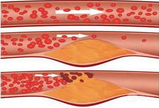
背景:尸检研究表明,脑淀粉样血管病(CAA)与认知功能障碍和痴呆发生风险相关。研究者分析前瞻性队列研究中CAA患者的神经心理学测验的数据,识别认知障碍的发病率及脑磁共振成像特点和载脂蛋白E基因相关性。
方法:数据来自34个CAA,16个阿尔茨海默病,69个轻度认知障碍,27个缺血性中风的参与者。神经心理测试结果表示为Z分数的测试手册提供的规范性数据,然后分为域的内存,执行功能和处理速度。
结果:CAA受试者平均测试分数的记忆功能(-0.44±1.03;P = 0.02),执行功能(-1.14±1.07;P<0.001)和处理速度(-1.06±1.12;P<0.001)显著低于正常人。27例CAA受试者(79%)有轻度认知障碍基于低认知能力伴随着认知问题。CAA的受试者和阿尔茨海默病有同样的低执行功能分数,但相对保存记忆。CAA受试者执行功能和加工速度的得分均低于缺血性脑卒中。CAA患者较低的处理速度与较高的磁共振成像的脑白质高信号量相关。与载脂蛋白Eε4等位基因没有相关性。
结论:CAA患者轻度认知功能障碍是很普遍的。CAA的总体认知特征更类似于血管性认知障碍而不是阿尔茨海默病。脑白质缺血性病变可能基于CAA处理速度受损。
原始出处:
Case NF, Charlton A, et al. Cerebral Amyloid Angiopathy Is Associated With Executive Dysfunction and Mild Cognitive Impairment. Stroke. 2016 Jun 23.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#血管病#
33
学习了,好文值得点赞!
66
#轻度认知功能障碍#
44
#功能障碍#
35
学习了,方法学不错,思路不错
75