CohBar发现CXCR4的新型肽抑制剂,CXCR4是肿瘤生长和转移的关键调节因子
2020-01-09 不详 MedSci原创
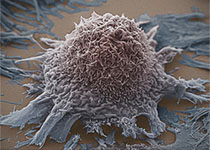
CohBar是一家临床阶段生物技术公司,致力于开发基于线粒体的疗法(MBT)来治疗慢性疾病并延长寿命。该公司发现了一系列新型的线粒体肽类似物,它们具有强大的体外活性,可作为CXC趋化因子受体4型(CXCR4)的选择性抑制剂,并且在黑素瘤小鼠模型中具有初步的体内功效。CXCR4是涉及肿瘤生长,侵袭,血管生成,转移和对治疗的抵抗力的关键调节受体。
CohBar是一家临床阶段生物技术公司,致力于开发基于线粒体的疗法(MBT)来治疗慢性疾病并延长寿命。该公司发现了一系列新型的线粒体肽类似物,它们具有强大的体外活性,可作为CXC趋化因子受体4型(CXCR4)的选择性抑制剂,并且在黑素瘤小鼠模型中具有初步的体内功效。CXCR4是涉及肿瘤生长,侵袭,血管生成,转移和对治疗的抵抗力的关键调节受体。
线粒体编码肽(MBT5)的新型肽类似物是在细胞实验中证明了对人CXCR4受体的有效和选择性抑制,其IC50值在低纳摩尔浓度范围内。在体内难以治疗的黑色素瘤小鼠模型B16F10同基因肿瘤模型中,MBT5类似物与替莫唑胺联合皮下给药显示出增强的抗肿瘤活性,与对照组相比,在11天后肿瘤生长减少了61%,单用替莫唑胺使肿瘤的生长仅减少了38%。
CohBar计划在其他动物模型中进一步探索该新肽家族的功效,以鉴定出新的临床开发MBT候选物。
CXCR4在超过75%的癌症中过表达,高水平的受体与不良的预后相关。已表明抑制CXCR4受体可动员免疫细胞,增强化学疗法和免疫疗法在各种癌症中的作用,并减少转移性肿瘤的发展。CXCR4还调节骨髓中造血干细胞和恶性细胞的归巢和保留。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#HbA#
41
#抑制剂#
36
#肿瘤生长和转移#
21
#调节因子#
36
#CXCR4#
41