J Matern Fetal Neonatal Med:分娩方式对早产新生儿结局的影响
2021-07-15 MedSci原创 MedSci原创
在过去的20年中,剖腹产的比例有所上升。在34周以下的分娩中(占分娩总数的2.75%),剖腹产率为50%。在过去,人们认为CD可以减少早产儿的新生儿死亡和出生时的创伤,然而,现在对早产儿的最佳分娩方式
在过去的20年中,剖腹产的比例有所上升。在34周以下的分娩中(占分娩总数的2.75%),剖腹产率为50%。在过去,人们认为CD可以减少早产儿的新生儿死亡和出生时的创伤,然而,现在对早产儿的最佳分娩方式仍有争议。一些作者发现,CD与呼吸道发病率的增加有关,尤其是早产新生儿。另一方面,一些研究表明,CD与新生儿发病和死亡的风险降低有关。其他研究发现,CD和阴道分娩(VD)在新生儿结局上没有明显差异。近日,一项回顾性队列研究评估了分娩方式对妊娠34周前出生的新生儿结局的影响,研究结果已发表于J Matern Fetal Neonatal Med。

研究纳入2009年1月至2017年7月期间妊娠24.1至34.0周之间出生的所有单胎活产新生儿,比较了阴道分娩(VD)和剖腹产(CD)的母体和妊娠特征以及新生儿结局。
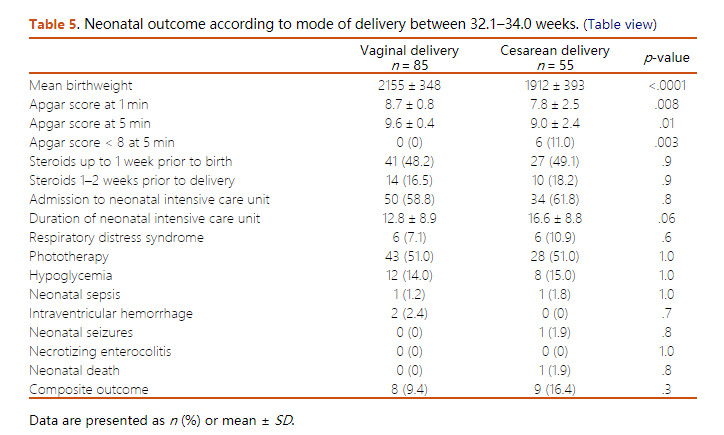
结果显示,在475例早产儿中,223例(46.9%)是阴道分娩,252例(53.1%)是剖腹产。与CD分娩的产妇相比,阴道分娩的产妇更年轻(29.6±6岁vs. 31.2±6岁,p=0.003),高血压疾病(9.9 vs. 36.1%,p<0.001)和糖尿病(0.4 vs. 4.4%,p=0.006)的比例更低,药物滥用的比例更高(4.9 vs. 1.6%,p=0.006)。与CD出生的新生儿相比,VD出生的新生儿有更高的出生体重(1716±595 vs. 1443±507,p < .001),更少的小胎龄率(7.2 vs. 19.4%,p < .001)。虽然VD新生儿的Apgar评分比CD高,但两种分娩方式的新生儿综合结果相似。这些发现在根据胎龄(GA)进行的亚组分析中是一致的。逻辑回归分析显示,只有在分娩前1周使用倍他米松(aOR = 0.59,95% CI 0.38-0.92,p = .001)和分娩时的GA(aOR = 0.74 95% CI 0.64-0.84,p = .004)对新生儿综合结局有独立保护作用。
综上,该研究结果表明,新生儿的结局似乎不受分娩方式的影响。
原始出处:
Ohad Gluck, et al., The impact of mode of delivery on neonatal outcome in preterm births. J Matern Fetal Neonatal Med. 2021 Apr;34(8):1183-1189. doi: 10.1080/14767058.2019.1627319.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#分娩方式#
37
#Nat#
50
#Neon#
55
#分娩#
54
#ATA#
48
#Med#
44