GUT:治疗内皮功能障碍的新方法!
2017-04-06 MedSci MedSci原创
内皮功能障碍是心血管疾病的早期关键标记,近期,一项发表在杂志GUT上的研究旨在评估益生元对内皮功能障碍的有益作用,此项研究在脂肪变性和内皮功能障碍的原始小鼠模型中进行。此项研究评估了肠内微生物群对血管功能障碍的影响,使用载脂蛋白E敲除(Apoe - / - )小鼠,喂食小鼠n-3多不饱和脂肪酸(PUFA)12周,于最后的15天予以或不予以菊粉型果聚糖(ITF)。分离肠系膜和颈动脉以评价内皮依赖性松
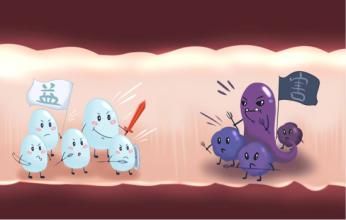
内皮功能障碍是心血管疾病的早期关键标记,近期,一项发表在杂志GUT上的研究旨在评估益生元对内皮功能障碍的有益作用,此项研究在脂肪变性和内皮功能障碍的原始小鼠模型中进行。
此项研究评估了肠内微生物群对血管功能障碍的影响,使用载脂蛋白E敲除(Apoe - / - )小鼠,喂食小鼠n-3多不饱和脂肪酸(PUFA)12周,于最后的15天予以或不予以菊粉型果聚糖(ITF)。分离肠系膜和颈动脉以评价内皮依赖性松弛性能。评估盲肠微生物群组成(16S rRNA基因的Illumina测序)以及参与控制血管功能的关键途径/介质,包括胆汁酸(BA)分析,肠和肝脏关键基因的表达,一氧化氮和肠激素的产生。
此项研究结果显示:补充ITF可以通过一氧化氮(NO)合酶/ NO途径的激活,完全逆转n-3 PUFA缺失的Apoe - / - 小鼠的肠系膜和颈动脉内皮功能障碍。由益生元处理引起的肠道微生物群变化包括产生NO细菌的增加。肠道和肝脏基因表达的变化也发生在ITF组,表明胰高血糖素样肽1的产生和BA转化可以作为内皮功能保存的驱动因素。
此项研究首次证明ITF能够改善内皮功能障碍,暗示肠道微生物群和肠道肽的短期适应性。如果能够在人体中得到证实,益生元可以作为预防代谢紊乱相关心血管疾病的一种新方法。
原始出处:
Catry E, Bindels LB, et al. Targeting the gut microbiota with inulin-type fructans: preclinical demonstration of a novel approach in the management of endothelial dysfunction. Gut. 2017 Apr 4. pii: gutjnl-2016-313316. doi: 10.1136/gutjnl-2016-313316.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#内皮功能障碍#
45
#新方法#
41
#功能障碍#
42
#内皮功能#
36
反复实践,反复学习,认真推敲,不断提高自己的业务水平。
69