BJH:地塞米松介导的 Notch 信号抑制阻断了白血病和间充质基质细胞的相互作用
2021-11-23 MedSci原创 MedSci原创
急性髓系白血病 (AML) 是一种血液系统恶性肿瘤,其特征是预后不良。骨髓间充质基质细胞 (BM MSC) 支持白血病细胞预防化疗诱导的细胞凋亡。
急性髓系白血病 (AML) 是一种血液系统恶性肿瘤,其特征是预后不良。骨髓间充质基质细胞 (BM MSC) 支持白血病细胞预防化疗诱导的细胞凋亡。地塞米松对涉及骨髓间充质干细胞和白血病细胞相互作用的复杂骨髓壁龛的影响以及这如何影响治疗结果没有研究。
因此,国外一研究团队试图对此进行调查,以提高对白血病 BM 生态位相关信号的理解,并最终确定新颖且有效的抗白血病治疗策略。在体外和体内详细研究了 AML 细胞与 BM MSC 的串扰分析以及如何在治疗水平上利用它们的相互作用。
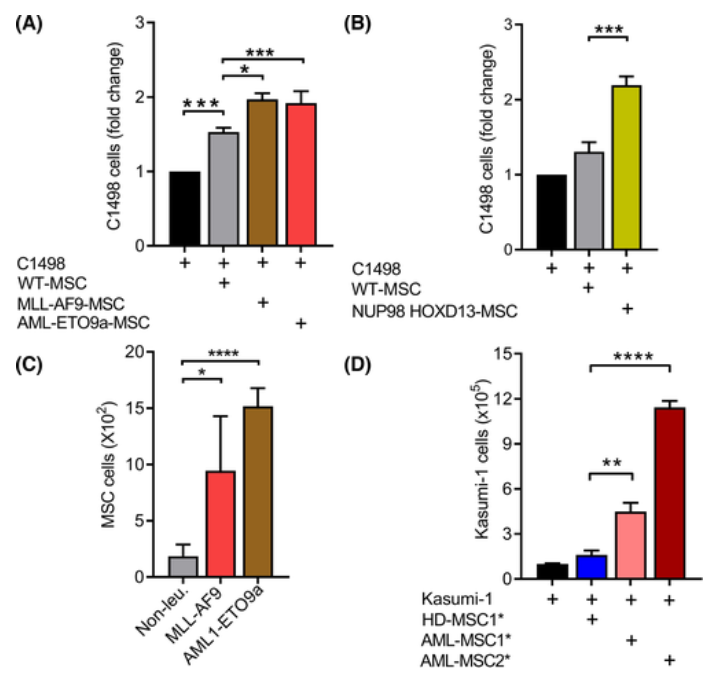
他们使用了先前所描述的鼠AML细胞系,C1498和MSCS从控制分离[野生型(WT)的MSC]和白血病小鼠(AML的MSC )。从模拟与AML1-ETO9a和MLL-AF9肿瘤融合蛋白(分别为 t(8;21)(q22;q22) 和 t(9;11)(p22;q23) 的产物)相关的人类 AML 亚型的小鼠中分离出 MSC 。将 C1498 细胞和 WT-/AML MSCs 直接接触或通过 transwell 插入物分开。与没有接受 MSC 支持的细胞相比,WT MSC 显着支持 C1498 细胞的增殖
鼠和人急性髓性白血病 (AML) 间充质基质细胞 (MSC) 支持白血病细胞的增殖
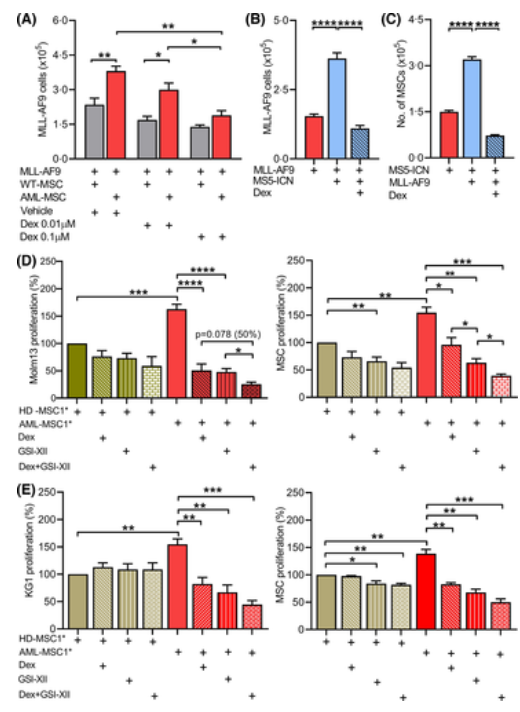
他们假设地塞米松介导的对 AML MSC 中 Notch 信号传导的阻断可能解释了在 AML 患者中观察到的治疗益处。为了验证假设,将MLL-AF9白血病细胞和 WT 或 AML MSC 共培养并用载体(磷酸盐缓冲盐水,PBS)或不同剂量的地塞米松处理。
地塞米松在体外对急性髓系白血病 (AML) 细胞和 AML-间充质基质细胞 (MSC) 相互作用的作用
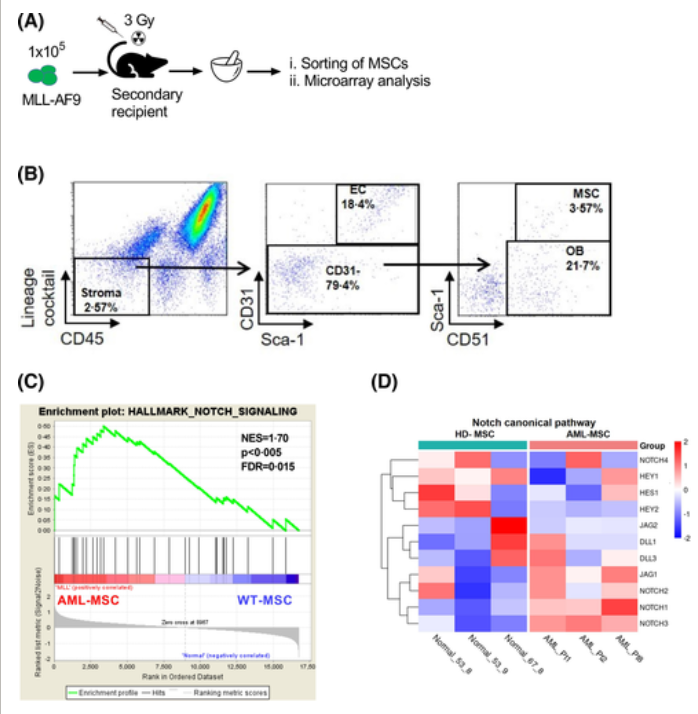
为了验证使用鼠 AML 细胞系 C1498 和原代鼠 MSC 获得的结果并证明结果不是特定于共培养系统的结果,她们使用了永生化人类 MSC 和人类 AML 细胞系 Kasumi-1,为了验证原代和永生化 MSC 的表型具有可比性,检查了它们的表面标志物和分化为脂肪细胞、软骨细胞和骨细胞的能力。为了在分子水平上表征 AML MSC,从非白血病(WT MSC)和MLL-AF9白血病小鼠中分选了 MSC,并使用 RNA 微阵列进行了基因表达谱分析。
急性髓性白血病 (AML) 间充质基质细胞 (MSC) 的分子特征
他们评估了地塞米松对MLL-AF9转基因白血病小鼠白血病进展和存活的治疗效果,以及地塞米松是否也影响了体内Notch 信号传导。移植了MLL-AF9-将白血病细胞表达到 C57BL/6 (WT) 小鼠中,随后每周一次施用 0·1 mg/kg 地塞米松或载体 (PBS)。
地塞米松对急性髓系白血病 (AML) 细胞和 AML-间充质基质细胞 (MSC)体内相互作用的作用
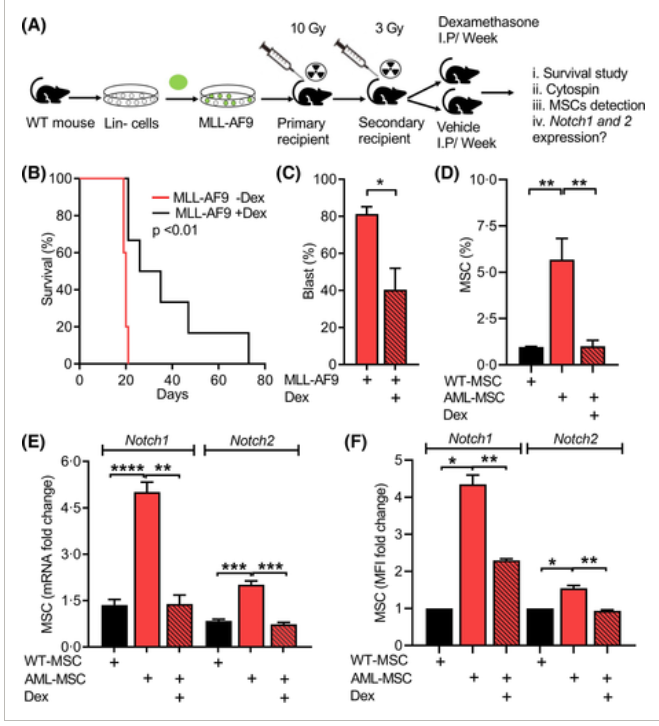
他们的数据,特别是在 AML MSC 中,证明了 Notch 标志基因集的富集和 Notch 信号传导的激活。在治疗上,地塞米松治疗消除了白血病细胞和 AML MSC 的相互作用并阻断了 Notch 信号传导。Notch抑制剂(GSI-XII)进一步增强了地塞米松的治疗效果。
地塞米松治疗干扰的白血病和急性髓系白血病(AML)-间充质基质细胞(MSC)相互作用
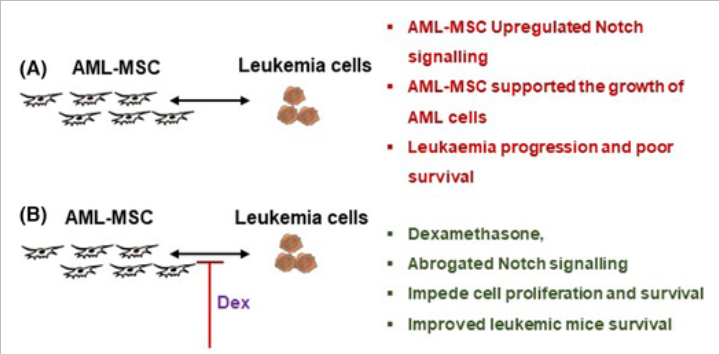
研究证明了源自白血病的 MSC (AML MSC) 和健康供体 (HD MSC) 之间的功能差异。白血病和 AML 间充质干细胞的直接相互作用对于影响 AML 细胞增殖是必不可少的。进一步确定了 Notch 表达及其在 AML MSC 中激活的重要作用,有助于增强 AML 细胞的增殖。AML MSC中细胞内Notch结构域(Notch ICN)的过表达增强了AML细胞的增殖。从治疗的角度来看,地塞米松治疗阻碍了 AML MSC 中的 Notch 信号传导,导致 AML 细胞增殖减少。
同时,Notch 抑制剂仅对白血病细胞有轻微影响,但强烈影响了 AML MSC 中的 Notch 信号传导并取消了它们对 AML 细胞的细胞保护功能。在体内,地塞米松治疗阻碍了 AML MSC 中的 Notch 信号传导,导致 AML MSC 数量减少并提高了白血病小鼠的存活率。
总之,使用地塞米松或 Notch 抑制剂靶向白血病细胞和 AML MSC 的相互作用可能会进一步改善 AML 患者的治疗结果。
原始出处:
Ahmed, H.M.M., Nimmagadda, S.C., Al-Matary, Y.S., Fiori, M., May, T., Frank, D., Patnana, P.K., Récher, C., Schliemann, C., Mikesch, J.-H., Koenig, T., Rosenbauer, F., Hartmann, W., Tuckermann, J., Dührsen, U., Lanying, W., Dugas, M., Opalka, B., Lenz, G. and Khandanpour, C. (2021), Dexamethasone-mediated inhibition of Notch signalling blocks the interaction of leukaemia and mesenchymal stromal cells. Br J Haematol. https://doi.org/10.1111/bjh.17940
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#阻断#
39
#相互作用#
0
#基质#
36
#Notch#
33
#互作#
27
#OTC#
25
不错
43