Cardiovasc Res: 我们要更加关注右心衰竭-转录因子Hand2
2021-09-24 刘少飞 MedSci原创
与肺动脉高压相关的右室衰竭使3 年内的长期生存率降低至55%,与左心室 (LV) 相比,右心室 (RV) 衰竭的病理生理学研究仍落后于相关的高死亡率和发病率。
众所周知,左心室 (LV) 相比,右心室 (RV) 衰竭的病理生理学研究仍落后于相关的高死亡率和发病率。心力衰竭 (HF),简单描述为心脏无法泵血,是全球发病和死亡的主要原因,目前影响超过 2600 万人。 通常,HF 分为左心室 (LV) 和右心室 (RV) 衰竭,具体取决于哪个心室衰竭。 大多数研究都集中在 LV 衰竭上,而 RV 衰竭较少受到关注。 因此,LV 衰竭的知识比 RV 衰竭的知识更多、更准确也就不足为奇了。 同样,大多数 HF 疗法都针对 LV,并且通常也用于患有 RV 衰竭的患者。 由于 RV 衰竭仍然与不良预后相关,因此迫切需要新的 RV 特异性疗法。
近日,由荷兰学者P. A. da Costa Martins教授团队的新研究发表在Cardiovasc Res,其
研究题目:The adult heart requires baseline expression of the transcription factor Hand2 to withstand RV pressure overload.
期刊年卷:Cardiovasc Res 2021 Sep 22;
通讯作者:P. A. da Costa Martins,Department of Molecular Genetics, Faculty of Sciences and Engineering; CARIM School for Cardiovascular Diseases, Faculty of Health, Medicine and Life Sciences; Maastricht University, Maastricht, Netherlands.

课题组之前的研究发现,胚胎基本螺旋-环-螺旋转录因子心脏和神经嵴衍生物表达-2(Hand2)在成人心脏中重新表达,并激活“胎儿基因程序”,有助于在 LV 压力超负荷条件下病理性心脏重塑。本研究的目的是为了了解 Hand2 对 RV 重塑的作用。
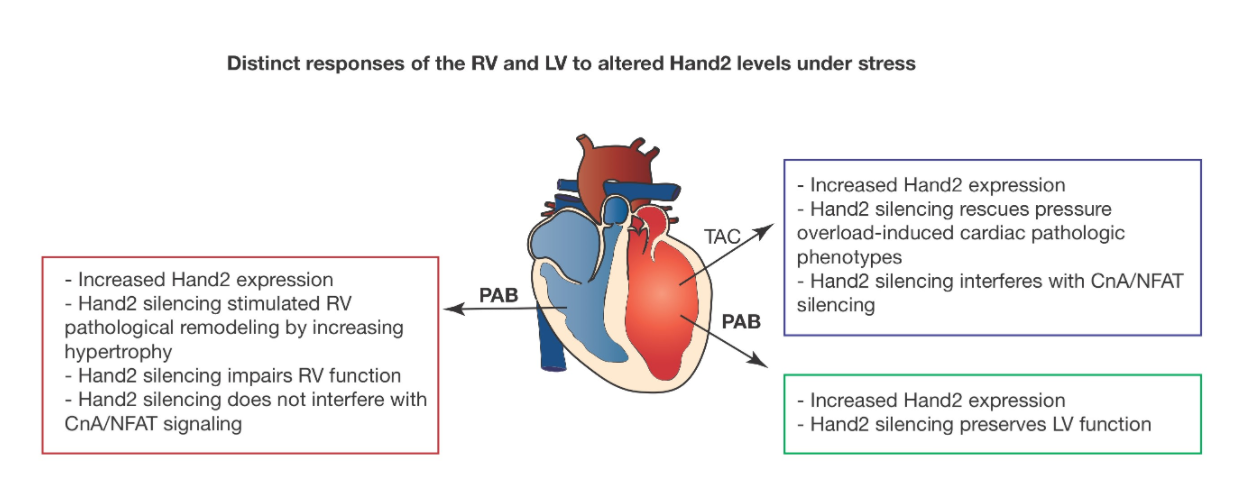
研究使用转基因小鼠Hand2F/F 和 MCM-Hand2F/F,经他莫昔芬(分别为对照和敲除)处理,手术进行肺动脉缩窄术(PAB)诱导RV 压力超负荷6周 。评估所有实验组的超声心动图和 MRI 衍生的血流动力学参数以及分子重塑,并与假手术对照进行比较。随着这些小鼠出现更肥大和更严重的心脏功能障碍,Hand2 耗竭似乎使 RV 对压力超负荷更敏感。与此同时,来自肺动脉高压患者的人类心脏的 RV 样本中也观察到 Hand2 的更高表达水平。反过来,RV 压力超负荷心脏的 LV 也受到显着影响,表现为形状变化、LV 质量减少和心脏功能受损。 RNA 测序揭示了一组不同的基因,与之前描述的压力过载 LV 相比,这些基因在压力过载 RV 中失调。
研究启示,与肺动脉高压相关的右室衰竭使3 年内的长期生存率降低至55%,这表明诊断后3 年几乎有一半的患者将死亡。为了使肺动脉高压的患者受益,需要适当的 RV 特异性治疗。该研究工作表明,当前的治疗方法和 LV 衰竭的潜在机制可能不适合 RV 衰竭。虽然 Hand2 缺失有利于 LV 对压力的反应,但它在类似条件下对 RV 尤其有害,因此,突出了不区分治疗目标或治疗 RV 或 LV 衰竭的潜在严重后果。在 RV 压力超负荷的情况下,Hand2 的心脏特异性耗竭与严重的心功能不全有关。虽然抑制 Hand2 表达可以预防 LV 压力超负荷条件下的心脏功能障碍,但同样不适用于 RV 压力超负荷条件。这项研究强调需要更好地了解驱动 RV 与 LV 病理重塑的分子机制,以便更好地诊断和治疗 RV 或 LV 衰竭患者。
原文出处:
R F Videira, The adult heart requires baseline expression of the transcription factor Hand2 to withstand RV pressure overload, Cardiovascular Research, 2021;, cvab299, https://doi.org/10.1093/cvr/cvab299
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#右心衰竭#
51
#转录#
30
#心衰竭#
32
#右心衰#
37
#ASC#
29
#心衰#这项研究强调需要更好地了解驱动 RV 与 LV 病理重塑的分子机制,以便更好地诊断和治疗 RV 或 LV 衰竭患者。
74
#转录因子#
28
很好
51
不错,学习了
46