Front Endocrinol:丙基硫氧嘧啶和甲巯咪唑治疗Graves病对血管粥样硬化标志物的不同影响
2022-01-13 从医路漫漫 MedSci原创
甲状腺功能亢进症是一种体内促甲状腺激素(TSH)水平低和甲状腺激素水平高的疾病;Graves病是导致这种疾病的最常见的原因。
背景:甲状腺功能亢进症是一种体内促甲状腺激素(TSH)水平低和甲状腺激素水平高的疾病;Graves病是导致这种疾病的最常见的原因。甲状腺功能亢进症会导致高水平的身体新陈代谢,经常会引发心力衰竭等并发症。最近的研究发现甲状腺功能亢进与动脉粥样硬化性心血管疾病(ASCVD)有潜在的相关性。游离T4(FT4)与ASCVD相关,与其他心血管风险无关,如血脂异常、肥胖和心房颤动。鉴于ASCVD是全球最主要的死亡原因,其早期发现值得研究,尤其是在甲亢患者中。
Graves病ASCVD的发病机制与自身免疫性疾病的炎症效应有关,也与过量甲状腺激素的作用有关。这种情况会导致血管动脉粥样硬化。血管动脉粥样硬化可以通过黏附分子如细胞间黏附分子-1(ICAM-1),血管细胞黏附分子-1(VCAM-1)和E-选择素-以及动脉硬度和厚度来测量,分别通过脉搏波速度(PWV)和颈动脉内膜中层厚度(CIMT)来测量。黏附分子是内皮激活的重要蛋白质,因为它们介导单核细胞和巨噬细胞在内皮细胞的黏附和迁移,表明血管对炎症的反应。同时,PWV和cIMT测量显示血管壁的结构和功能的改变。丙基硫氧嘧啶(PTU)和他巴唑除了具有抗甲状腺作用外,在预防Graves病动脉粥样硬化形成方面可能有不同的作用。
目的:探讨抗甲状腺药物对甲亢患者血管粥样硬化标志物的影响。
方法:本研究为随机单盲临床试验,于2019年6月至2020年7月在印度尼西亚雅加达综合医院进行,共36例Graves病患者。Graves病由甲状腺功能亢进合并弥漫性甲状腺肿的临床表现进行确诊,并行促甲状腺激素(TSH)、游离T4(FT4)和TSH受体抗体(TRAb)检测确诊。参与者随机分配到PTU或他巴唑治疗组,并随访3个月。以黏附分子[细胞间黏附分子-1(ICAM-1)、血管细胞黏附分子-1(VCAM-1)和E-选择素]、颈动脉硬度[脉搏波速度(PWV)]和厚度[颈动脉内膜中层厚度(CIMT)]代表动脉粥样硬化的标志物。
结果:研究结束时,24名参与者达到甲状腺功能正常(PTU组13人,他巴唑组11人)。随访3个月后,PTU组ICAM-1[治疗前:204.1(61.3vs.141.6)ng/ml;p=0.001]、VCAM-1[837vs.510vs.510(402-630)ng/ml;p<0.001]和E-选择素[32.1vs.28.2(21.636.8)ng/ml;p=0.045]均有明显改善。在他巴唑组,仅观察到血管细胞黏附分子-1的改善[725vs.472(367-590);p=0.001]。同时,我们发现两组的PWV和CIMT均无明显变化。

表1 抗甲状腺治疗3个月后血管粥样硬化标志物的变化。
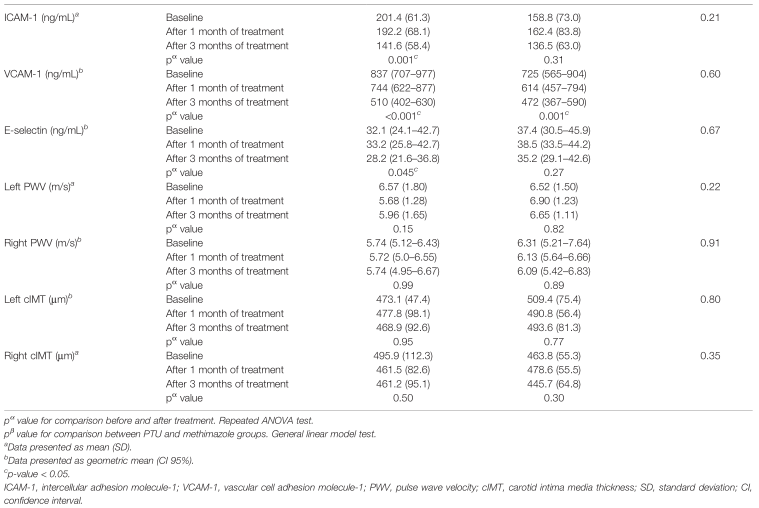
表2 PTU组和他巴唑组抗甲状腺治疗3个月后血管粥样硬化标志物的变化。

图1 黏附分子的变化:(A)ICAM-1;(B)VCAM-1;(C)E-选择素。经过3个月的抗甲状腺药物治疗。细胞间黏附分子1;VCAM-1血管细胞黏附分子-1。使用一般线性模型检验对比较进行评估。
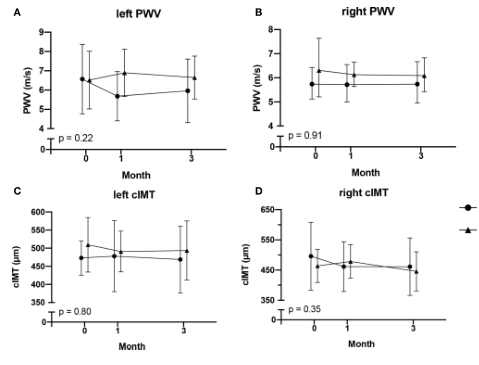
图2 PWV改变:(A)左PWV;(B)右PWV;及(C)左CIMT;(D)右CIMT。经过3个月的抗甲状腺药物治疗。脉搏波速度(PWV)、颈动脉内膜中层厚度(CIMT)。使用一般线性模型检验对比较进行评估。

图3 PTU和甲巯咪唑在Graves病动脉粥样硬化病理生理学中的作用机制。AKT,蛋白激酶B;NF-kB,核因子kappa B;IKK, IKb激酶;PI-3K,磷酸肌醇3-kinase;PTEN、磷酸酶和张力蛋白同源物;丙基硫氧嘧啶PTU;ROS,活性氧;细胞间粘附molecule-1;VCAM-1,血管细胞粘附分子-1。甲状腺激素诱导PI-3K/AKT/IKK/NF-kB通路的激活,进而增加黏附分子- icam -1、VCAM-1和e -选择素的表达。此外,甲状腺激素还可增加ROS,通过IKK增强NF-kB的激活。而PTU可以通过诱导PTEN的表达来阻断PI-3K/AKT/IKK/NF-kB通路,PTEN是一种可以阻断PI-3K/AKT通路的抑癌基因,导致黏附分子表达减少。
结论:抗甲状腺药物治疗能改善Graves病患者的黏附分子,但他巴唑的影响较小,而PWV和cIMT无明显变化。与他巴唑相比,PTU在改善黏附分子方面可能有更好的作用。
原文出处:
Wisnu W, Alwi I, Nafrialdi N,et al.The Differential Effects of Propylthiouracil and Methimazole as Graves' Disease Treatment on Vascular Atherosclerosis Markers: A Randomized Clinical Trial.Front Endocrinol (Lausanne) 2021;12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Graves#
44
#粥样硬化#
49
#标志物#
33
整挺好👍👍👍
63
#Graves病#
58