JAHA:绝经年龄、肥胖和心力衰竭发生率之间的关系
2022-04-14 MedSci原创 MedSci原创
随着肥胖状况的恶化,与体重指数和腰围较低的女性相比,这些患者发生心衰的风险显著增加,特别是在那些≥55岁绝经的女性。
更年期已经成为女性患心血管疾病(如心力衰竭)的一种特定危险因素。尽管既往研究报道早期绝经(绝经年龄小于45岁)与心衰有关。关于晚期绝经、55岁以上绝经对心衰发病率的影响尚未明确。肥胖对绝经年龄和心衰发病率之间关系的影响也未明确。绝经年龄与心力衰竭(HF)发病率之间的联系机制尚存争议。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在调查肥胖对绝经年龄和心衰发病率之间关系的异质性。

研究人员使用参加社区动脉粥样硬化风险研究随访的绝经后妇女,并使用Cox比例风险模型估计与绝经年龄相关的心力衰竭发生率。此外,研究人员评估了肥胖对效应的调整作用,并调整了心力衰竭的危险因素。绝经年龄分为:<45岁、45~49岁、50~54岁、≥55岁。
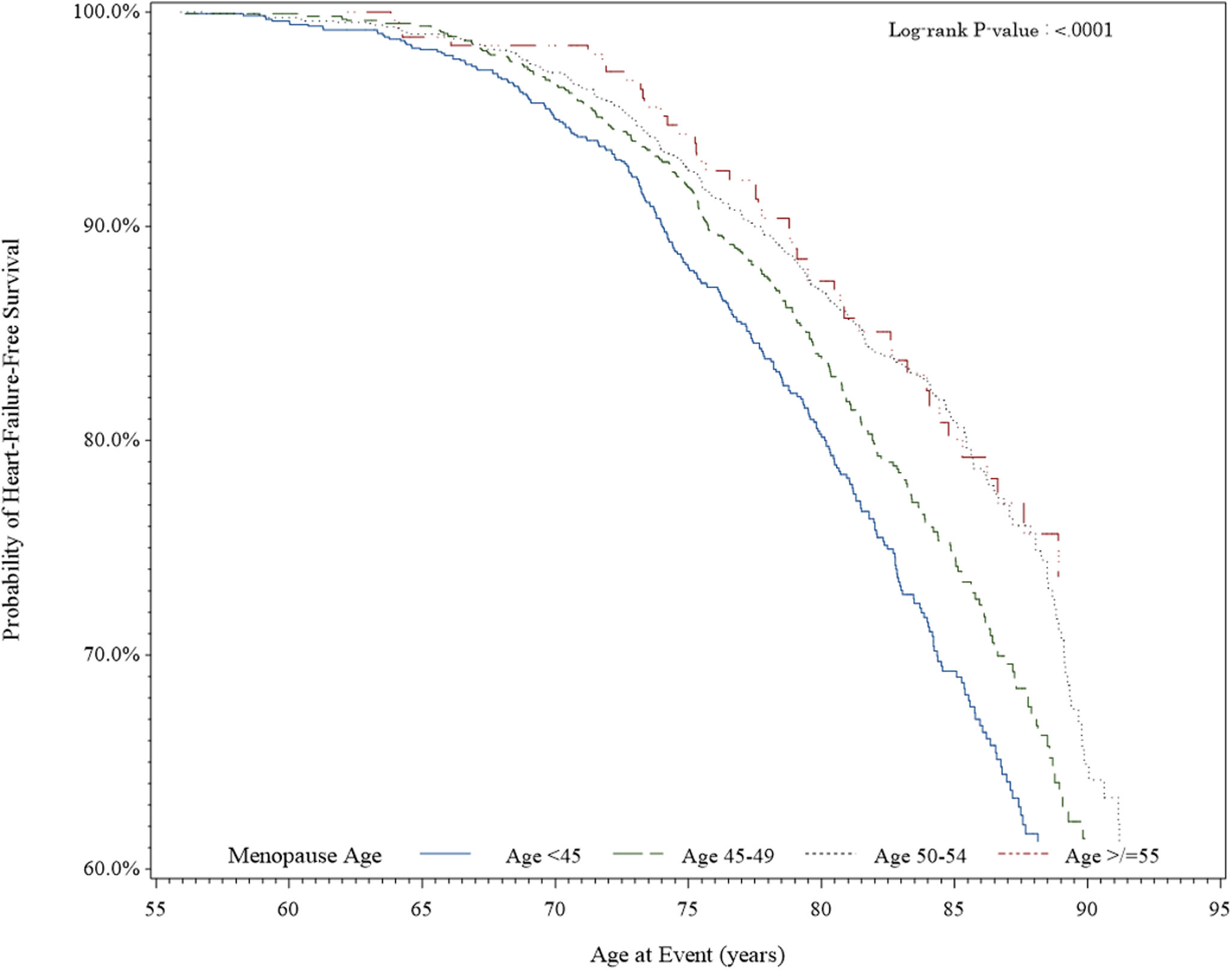
4441名绝经后妇女(年龄为63.5±5.5岁)在平均16.5年的随访中发生了903起HF事件。在≥55岁绝经的女性中,全身性肥胖和中心性肥胖发生率最高:分别为11.09人/1000人-年和7.38人/1000人-年。绝经年龄与体重指数和腰围在HF发病率上有显著的交互作用,交互作用P分别为0.02和0.001。在绝经年龄小于45岁的妇女中,体重指数增加导致心力衰竭的风险比升高[1.39, (1.05-1.84)];45-49岁[1.33,(1.06-1.67)];≥55岁[2.02,(1.41-2.89)]。仅在绝经年龄≥55岁的女性中,腰围增加导致心力衰竭的风险比升高[2.93,(1.85-4.65)]。
由此可见,随着肥胖状况的恶化,与体重指数和腰围较低的女性相比,这些患者发生心衰的风险显著增加,特别是在那些≥55岁绝经的女性。
原始出处:
Imo A. Ebong,et al.Relationship Between Age at Menopause, Obesity, and Incident Heart Failure: The Atherosclerosis Risk in Communities Study.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.024461
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#绝经年龄#
40
#发生率#
38
#绝经#
40
#AHA#
37
学习
49