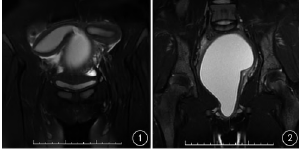
双子宫、双阴道畸形合并子宫腺肉瘤一例
2019-11-29 邵硕 郑宁 刘文娟 临床放射学杂志
患者女,17岁。因阴道分泌物6个月余,加重伴阴道突出物1周入院。14岁初潮,月经规律,月经量中等。妇科检查:外阴发育正常,处女膜孔呈圆形,用力时见处女膜孔处约1 cm紫红色息肉样物突出。直肠腹部诊:直肠黏膜光滑,进指顺利,扪及盆腔偏右侧直径约5 cm包块,边界欠清,活动差,与子宫分界不清。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#双阴道畸形#
27
#双子宫#
24
#畸形#
34
最后治疗方案呢
86