JAMA Cardiol:多形性室速患者服用β受体阻滞剂治疗的预后
2022-04-04 Nebula MedSci原创
与纳多洛尔相比,选择性β-受体阻滞剂与儿茶酚胺型多形性室性心动过速患者发生危及生命的心律失常事件风险升高相关
儿茶酚胺型多形性室性心动过速 (CPVT) 患者尽管使用了β-受体阻滞剂治疗,仍可能发生危及生命的心律失常事件 (LTAE)。对于这类患者,植入式心律转复除颤器(CPVT)的必要性一直广受争议。
本研究旨在探索RYR2型CPVT患者只采用β-受体阻滞剂治疗的长期预后,和采用ICD治疗的成本效益比。
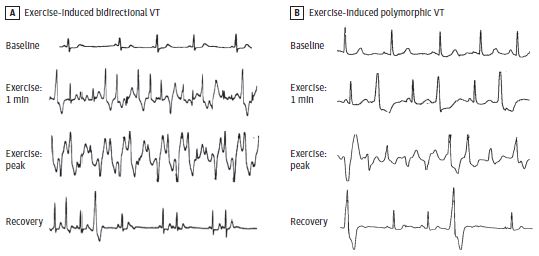
两例多形性室性心动过速患者不同状态下的心电图
这是一项回顾性队列研究,纳入了自1988年11月至2020年10月期间于ICS Maugeri医院分子心脏病诊所就诊的患者。本次分析纳入了携带RYR2致病性或可能致病性突变的且有长期临床随访数据的CPVT患者。受试患者仅采用选择性或非选择性β-受体阻滞剂治疗,并在有需要时植入ICD。主要终点是首次危及生命的心律失常事件(心源性猝死、心脏骤停、血流动力学不稳定的室性心动过速)。
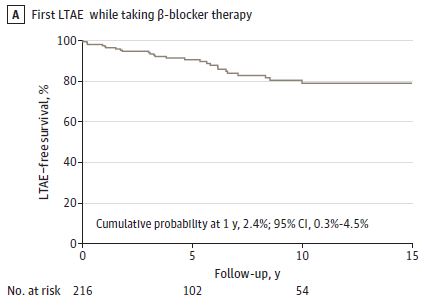
服用β-受体阻滞剂期间的无LTAE生存率
该队列共包含216位RYR2型CPVT患者(其中121位女性[55%],中位年龄14岁)。平均随访了9.4年,所有患者在随访期间只服用β-受体阻滞剂,有28位(13%)患者在确诊前经历了一次LTAE(年发生率 1.9%)。在多变量分析中,经历一次LTAE(风险比[HR] 3.3,p=0.02)或确诊前晕厥(HR 4.5,p=0.001)和携带C-末端结构域变异(HR 18.1, p<0.001)均与服用β-受体阻滞剂期间LTAE风险增加相关。
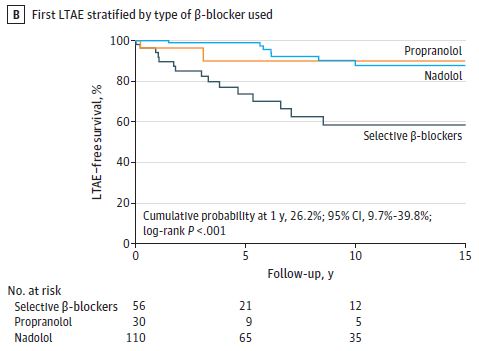
服用不同β-受体阻滞剂期间的无LTAE生存率
与纳多洛尔相比,服用选择性β-受体阻滞剂的患者发生LTAE的风险增加了6倍(HR 5.8,p=0.001)。相反,服用普萘洛尔和纳多洛尔的患者之间则无显著差异(HR 1.8, p=0.44)。
有79位(37%)患者植入了ICD,平均随访了8.6年。在LTAE发生时,ICD植入者比非ICD植入者更可能存活下来(100% vs 60%,p=0.01)。
总之,在该队列研究中,与纳多洛尔相比,选择性β-受体阻滞剂与CPVT患者的LTAE风险升高相关。独立于治疗,确诊前发生LTAE和晕厥以及C-末端结构域变异均是CPVT患者服用β-受体阻滞剂治疗失效的风险因素,ICD与高危CPVT患者的死亡率降低相关。
原始出处:
Mazzanti A, Kukavica D, Trancuccio A, et al. Outcomes of Patients With Catecholaminergic Polymorphic Ventricular Tachycardia Treated With β-Blockers. JAMA Cardiol. Published online March 30, 2022. doi:10.1001/jamacardio.2022.0219
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Cardiol#
31
#阻滞剂#
36
#受体阻滞剂#
29
#多形性#
35
#β受体阻滞剂#
34
#室速#
34