J Am Coll Surg:你知道直肠癌新辅助放化疗后多久做手术效果更佳吗?
2016-05-22 Seven L MedSci原创
nhideWhenUsed="false" Name="Medium Shading 1 Accent 5"/> <w:LsdException Locked="false" Priority="64" SemiHidden="false" UnhideWhenUsed="false" Name="Medium Shading 2 Accent 5"/> <w:LsdExcep
nhideWhenUsed="false" Name="Medium Shading 1 Accent 5"/>
先前有证据表明,局部晚期直肠癌患者接受新辅助放化疗(nCRT),有益于肿瘤体积的缩小,并改善患者长期的局部癌症控制情况。但是,患者完成新辅助放化疗后,应该间隔多长时间进行肿瘤切除术呢?间隔多长时间的手术才能最大限度的切除肿瘤、让病理降期呢?带着这个疑问杜克大学的研究者进行了一项研究。 该研究纳入了11760名II期和III期直肠腺癌患者,所有患者在接受nCRT后进行手术。最后一次放化疗时间到进行手术的时间,为研究中的“间隔时间”。该研究以手术切缘肿瘤细胞阳性与病理分期作为主要结局,此外研究者还评估了校正后间隔时间和研究终点的联系,并建立一个最佳的手术间隔时间阈值。
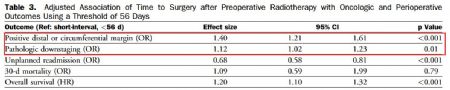
下图显示了间隔时间(横轴)与手术切缘肿瘤细胞阳性风险和病理分期下调可能性的联系。校正人口统计学、临床、肿瘤和治疗特点后,间隔时间为56天时,患者术中肿瘤的完全切除率和病理分期下调的可能性最高。 下图显示的为以56天为最佳手术间隔时间阈值时,不同时间间隔对肿瘤和围生期结局的影响。 间隔时间超过56天的患者,切缘肿瘤细胞阳性风险增加(OR=1.40, 95% CI 1.21 - 1.61, p < 0.001),病理分期下调的可能性下降(≥56天 vs. <56天, OR=1.12,
95% CI 1.02 - 1.23, p = 0.01)。 研究结果表明,局部晚期直肠癌患者新辅助放化疗后,间隔8周进行手术,可能是肿瘤最佳反应的临界阈值。 原始出处:
Zhifei Sun, Mohamed A. Adam,et al.Optimal Timing to Surgery after Neoadjuvant Chemoradiotherapy for Locally Advanced Rectal Cancer. J Am Coll Surg. 2016 Apr;222(4):367-7, 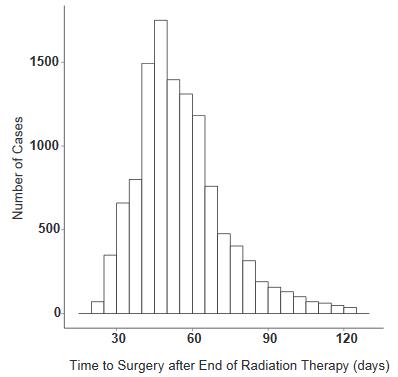

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#辅助放化疗#
30
#Coll#
32
拜读,好文
67
#新辅助#
28
#放化疗#
23
#新辅助放化疗#
34