心血管内科病例赏析——心肌梗死后频发室速
2018-01-18 MedSci MedSci原创
室性心动过速(VT)是指发生在希氏束分叉以下的束支、心肌传导纤维、心室肌的快速性心律失常 ,Wellens将其定义为:频率超过100次/min,连续3个或3个以上的自发性室性电除极活动,包括单形非持续性和持续性室性心动过速以及多形室性心动过速,如果是心脏电生理检查中心脏电刺激所诱发的室性心动过速,则必须是持续6个或6个以上的快速性心室搏动(频率>100次/min)。室性心动过速

室性心动过速(VT)是指发生在希氏束分叉以下的束支、心肌传导纤维、心室肌的快速性心律失常 ,Wellens将其定义为:频率超过100次/min,连续3个或3个以上的自发性室性电除极活动,包括单形非持续性和持续性室性心动过速以及多形室性心动过速,如果是心脏电生理检查中心脏电刺激所诱发的室性心动过速,则必须是持续6个或6个以上的快速性心室搏动(频率>100次/min)。室性心动过速可以起源于左心室及右心室,持续性发作时的频率常常超过100次/min,并可发生血流动力学状态的恶化,可能蜕变为室扑,室颤,导致心源性猝死 ,需要积极治疗。
病史:
患者为一50岁中年男性,患者6年前曾患“急性下壁及前壁心肌梗死”,当时未行溶栓、经皮冠状动脉介入治疗(PCI)等血运重建治疗。近1年患者无明显诱因反复发生心悸、胸闷、气短等症状,每次持续数分钟至半小时不等,不伴胸痛,可自行缓解。
于当地医院就诊,给予抗心律失常药物治疗,病情好转。近半个月心悸症状加重,共发作3次,每次持续数小时,气短、不能平卧,无黑曚及晕厥,给予静滴胺碘酮及口服β-受体阻滞剂,症状无明显改善,曾给予电复律转为窦性心律。现为求进一步诊治收入我科。患者自起病以来,神志清,精神差,饮食、睡眠可,二便无殊体重无明显改变。
查体:
患者神志清楚,精神一般,慢性病容,巩膜无黄染,双肺呼吸音清,未闻及干湿啰音,心率律不齐,偶有早搏。各瓣膜听诊区未闻及杂音;双肺底可闻及湿性啰音。腹软,腹部无压痛及反跳痛未触及包块,肝脾不大,无振水音,移动性浊音阴性,肠鸣音正常。四肢无殊,神经查体无殊。
辅助检查:
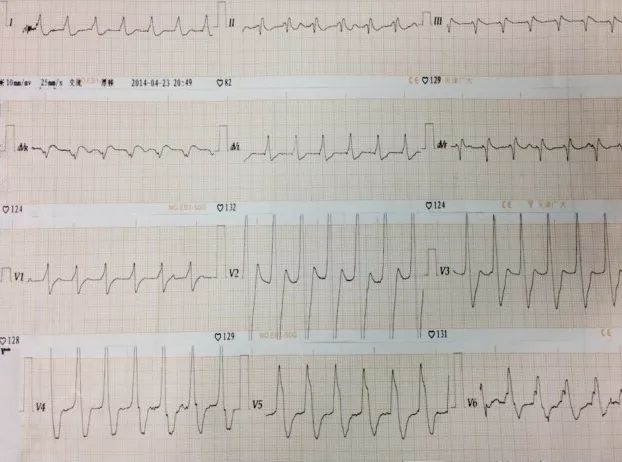
心电图(心悸发作时):宽QRS心动过速,考虑为室性心动过速。窦性心律,下壁及胸前导联病理性Q波。

心脏超声:左房和左室内径分别为45mm和77mm,射血分数0.43,左室后壁、下壁变薄,活动明显减弱,二尖瓣中到重度反流。
其他:Pro-BNP 4892 ng/ml、血清胆固醇6.8 mmol/L
简要解析:
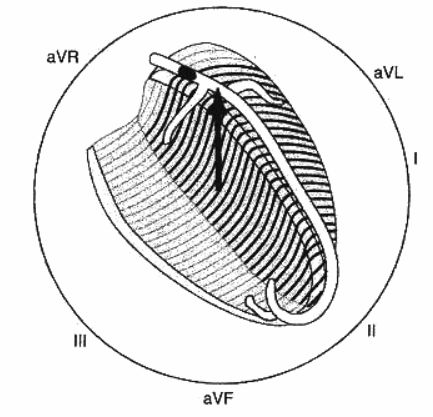
患者心肌梗死后6年频发室速,同时伴心功能不全,是ICD置入的适应证,但该患者室速发作频率慢,为120~130次/分,ICD可能识别较困难或无法识别,也可能将窦性心动过速伴差传误认为是室速引起不适当治疗,甚至误放电。当然,患者也可能发作快频率的室速或室颤,ICD置入是首选。对于目前发作的室速,导管消融更适合。因为心肌梗死后室速的发病机制较为清晰,为梗死心肌的瘢痕组织内部存在缓慢传导区,围绕瘢痕引起的折返性心动过速,消融缓慢传导区――峡部,可终止室速发作。在有经验的电生理中心,手术成功率在80%~90%之间。患者心功能不全,与心肌坏死、室速频繁发作、慢性缺血均密切相关,在消除室速后应积极进行血运重建,改善心肌供血,同时应行冠心病二级预防及慢性心衰长期药物治疗。
完整病例请前往【梅斯医生】→病例库→肝胆胰外科→“心悸、胸闷、气短1年,心悸加重半个月”
更多点评分析,趣味的学习,详情尽在梅斯医生上,您可以在这里体验模拟诊疗。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心血管内科#
23
#室速#
25
学习学习学习
64
学习了.获益匪浅!感谢分享
72