Gynecol Oncol:鳞状细胞癌抗原(SCC-Ag)是局部晚期宫颈癌患者的生存预后因素
2021-09-22 原艳妮 张师前 张师前公众号
Gynecol Oncol:鳞状细胞癌抗原(SCC-Ag)是局部晚期宫颈癌患者的生存预后因素
亮点
l SCC-Ag ≥1.2 ng/ml 是 LACC 患者的独立危险因素。
l 主动脉淋巴结受累是 LACC 患者的独立危险因素。
l SCC-Ag ≥1.2 ng/ml 的患者总体生存率较差。
l 晚期和对治疗的不完全反应是 LACC 患者的危险因素。
引言
自 1977 年首次描述鳞状细胞癌抗原 (SCC-Ag) 以来,一直被视为宫颈癌重要的生物标志物。SCC-Ag 是由正常宫颈鳞状上皮细胞表达的糖蛋白,在肿瘤发展过程中显着升高。28%-88%的宫颈鳞状细胞癌患者中血清 SCC-Ag 升高。
SCC-Ag 可用于评估患者对治疗的反应,随访和预判复发。SCC-Ag 的预后指导价值尚缺乏研究。本研究评估接受同步放化疗 LACC 患者 SCC-Ag 水平的预后价值,以及 SCC-Ag 水平的临界值。
材料和方法
多中心观察性回顾性研究包括 2000 年 8 月至 2016 年 12 月期间在西班牙八家三级转诊医院妇科肿瘤科管理的 LACC 患者。
所有患者均接受同步放化疗。
在初诊时评估患者治疗前电化学发光免疫测定法 SCC-Ag 水平。该试剂盒SCC-Ag 水平1.9 ng/ml 是正常上限。治疗结束后 3个月,通过体格检查、血浆 SCC-Ag 测量和 MRI 和/或 PET-CT 评估。阴道或宫旁区域的病变为局部复发;淋巴结转移(盆腔和/或主动脉)是区域性复发,其他部位为远端转移。
SPSS20.0 分析数据。卡方检验或 Fisher 精确检验进行变量比较。
结果
该研究包括 447 例患者,中位随访时间为53 个月,治疗前和治疗后 SCC-Ag 的中位水平分别为 3.4 ng/ml 和 0.8 ng/m。治疗前 SCC-Ag 的临界值为 11.75 ng/ml(敏感性 37.5%;特异性 80.5%),治疗后 SCC-Ag 的临界值为 1.24 ng/ml(敏感性 34.6%;特异性 83.1%)。在多变量 Cox 回归分析中,作为 OS 独立预测因子的因素是:FIGO 分期、主动脉旁淋巴结受累,治疗后 SCC-Ag 水平 ≥ 1.2 ng/ml和对治疗的不完全反应。

治疗前 SCC-Ag 水平≥11.7 ng/ml 的患者,平均生存时间为 138.63 个月;治疗前 SCC-Ag 水平 <11.7 ng/ml 的患者,则为 171.77 个月。治疗后 SCC-Ag 值≥1.2 ng/ml 的患者,平均生存时间为 126.6 个月;治疗后 SCC-Ag 值 <1.2 ng/ml 的患者,平均生存时间为 165.99 个月。
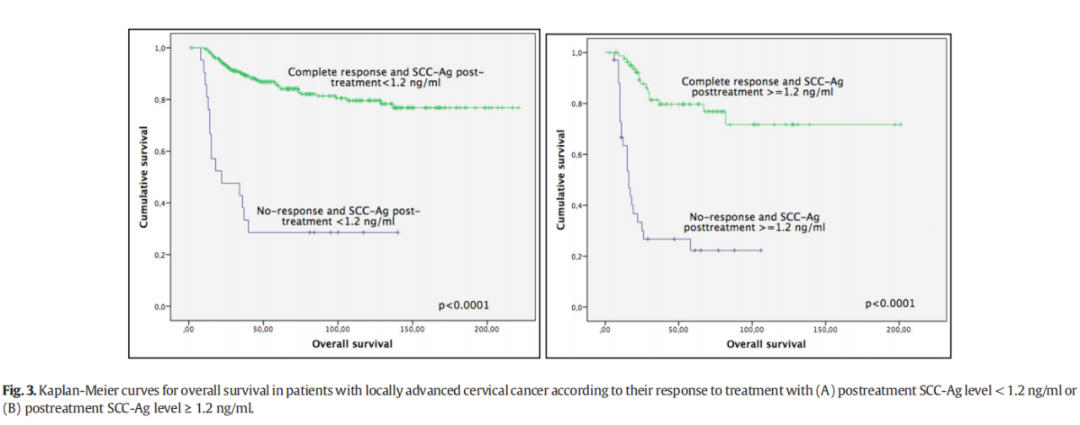
基于对治疗的反应和治疗后 SCC-Ag 水平,建立了四个 LACC 患者的预后组:完全缓解和治疗后 SCC-Ag <1.2 ng/ml 的患者,平均 OS 时间为 182.56 个月;完全缓解且治疗后 SCC-Ag ≥1.2 ng/ml 的患者,平均 OS 时间为 155.01 个月;不完全反应和治疗后 SCC-Ag <1.2 ng/ml 的患者,平均 OS 时间为 54.23 个月;不完全反应和治疗后 SCC-Ag ≥1.2 ng/ml 的患者,平均 OS 时间为 36.54 个月。
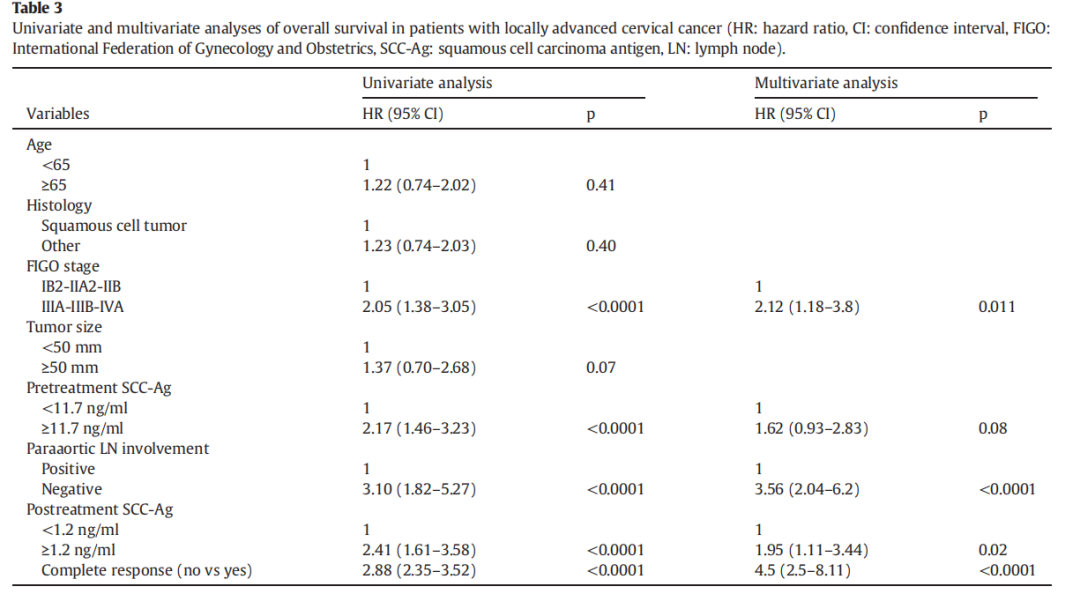
多变量 Cox 回归分析显示以下因素是 OS 的独立预测因素:FIGO 分期,主动脉旁淋巴结受累,治疗后 SCC-Ag 水平 ≥ 1.2 ng/ml和对治疗的不完全反应。
讨论
研究发现治疗后 SCC-Ag 水平是接受放化疗治疗LACC的独立预后因素。治疗终止后 3 个月 SCC-Ag 值≥1.2 ng/ml 的患者,总体生存率明显低于临界值较低的患者。
一项包括 559 例IB-IVA 期患者治疗后 SCC-Ag 水平的研究表明,临界值 1.8 ng/ml作为治疗失败的预测指标;多变量分析表明,治疗后 SCC-Ag 是复发的独立预后因素。Ryu团队评估了783 名 I-IV 期宫颈癌患者,发现治疗后 SCC-Ag 作为复发预测指标的最佳临界值为 0.9 ng/ml,多变量分析表明,治疗后 SCC-Ag 水平 >0.9 ng/ml 与较差的无病生存率显著相关。Kawaguchi等分析了 116 例LACC 患者(IIB-IVA 期),发现治疗后 SCC-Ag作为生存预测指标的最佳临界值水平为 1.15 ng/ml;多变量分析表明,治疗后 SCC-Ag 水平是生存的独立预后因素。另一项包括 401 例宫颈癌患者的研究中观察到,放疗后 2-3 个月持续升高的 SCC-Ag 水平较盆腔检查更能预测治疗失败,并与更高的宫颈癌发生远处转移率相关。因此,治疗后血浆 SCC-Ag 水平的评估可能有助于 LACC 患者的管理。
原始出处:
Benito V, Lubrano A, Pérez-Regadera JF, Torné A, Gil-Moreno A, Tejerizo-Garcia Á, Vergés R, Díaz-Feijoo B; SEGO Spain-GOG Group.Postreatment squamous cell carcinoma antigen as a survival prognostic factor in patients with locally advanced cervical cancer. A Spanish multicenter study. The SEGO Spain-GOG group.Gynecol Oncol. 2021 Aug;162(2):407-412
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#局部晚期#
33
#NEC#
38
#SCC#
43
#生存预后#
42
#细胞癌#
39
#Oncol#
27
#局部#
32
#宫颈#
26
#预后因素#
31
#晚期宫颈癌#
31