J Ophthalmol:健康人的施莱姆管和眼压在运动后可以正常恢复到运动前水平
2018-10-08 MedSci MedSci原创
华中科技大学同济医学院附属同济医院眼科的Li M和Yan X等近日在J Ophthalmol杂志上发表了一篇文章,他们观察了健康人运动后施莱姆管(SC)和眼压(IOP)的恢复过程。
华中科技大学同济医学院附属同济医院眼科的Li M和Yan X等近日在J Ophthalmol杂志上发表了一篇文章,他们观察了健康人运动后施莱姆管(SC)和眼压(IOP)的恢复过程。
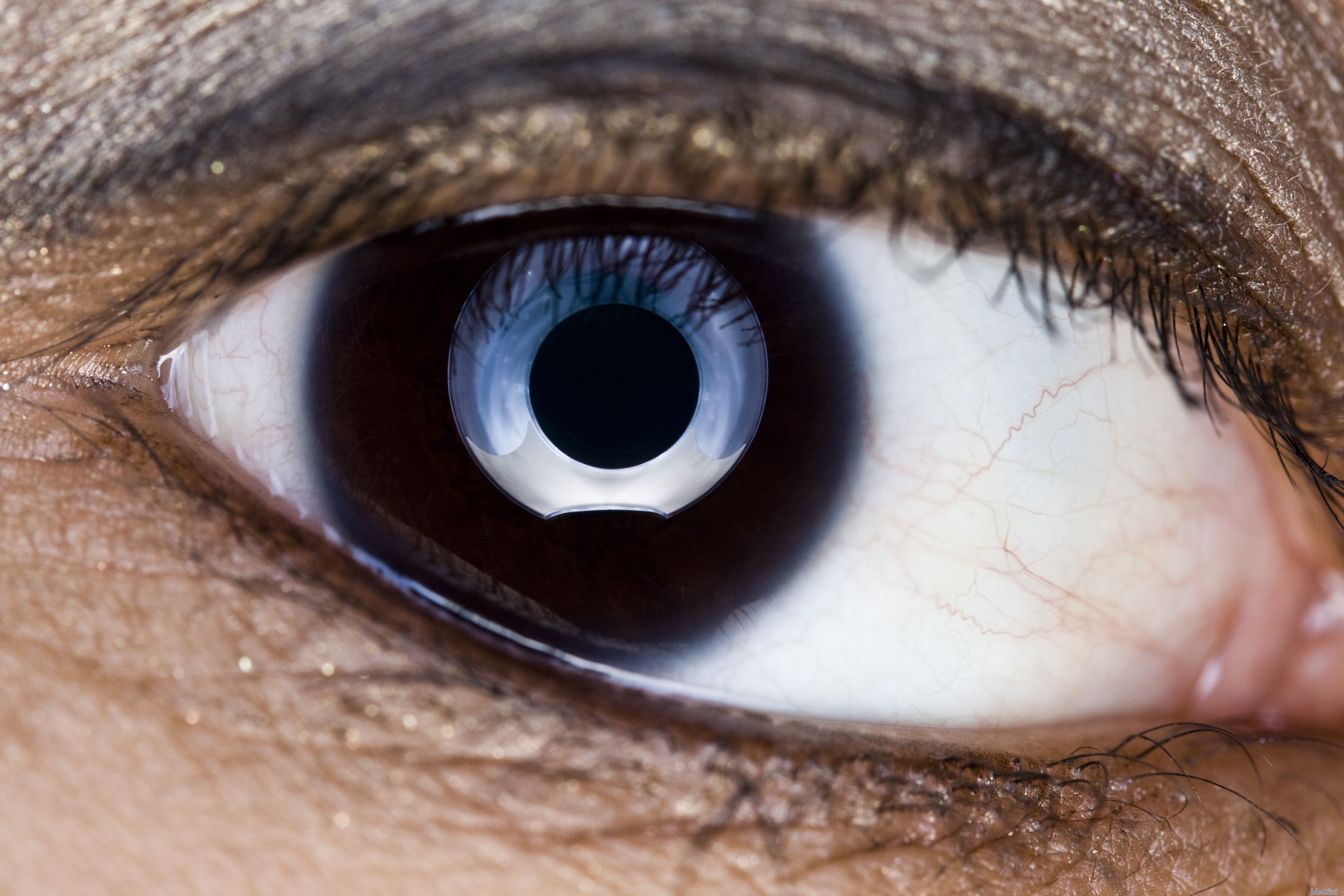
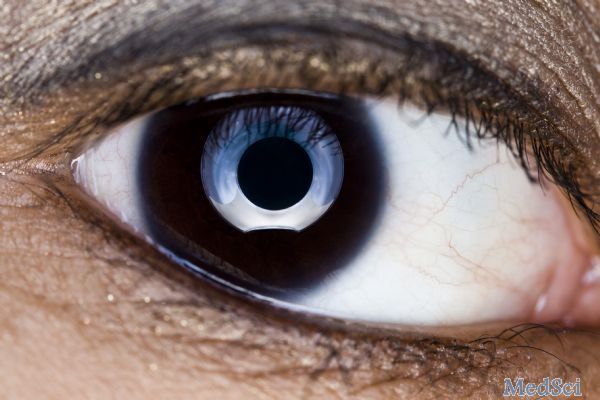
他们招募了20个健康个体。在运动前和运动后0、15、30和60分钟时评估SC和IOP。使用扫描光学相干断层扫描技术(SS-OCT)评估上、下、鼻象限和时间象限施莱姆管(SC)的情况。
结果他们发现,运动前后平均SC面积为3726.81±1167.06 vs. 4660.57±1284.82μm2,周长为324.11±58.95 vs. 367.19±73.34μm,运动后增加,运动期间IOP(14.02±2.33 vs. 11.65±1.90 mmHg)显着下降(所有p < 0.001)。运动后,SC和IOP均恢复至运动前的水平,运动后SC大小的的恢复时间为15分钟,短于眼压的恢复时间(60分钟)。在调整年龄、性别、眼轴长度、中央角膜厚度和球面等效后,运动后的SC尺寸的变化与运动后的IPO变化没有显着的相关性(均p> 0.05)。在运动前后SC比例也没有显着差异(均p> 0.05)。
因此,他们认为,运动诱导的SC扩张和眼压降低,在运动后可以恢复到运动前的水平,并且SC比IPO先恢复到运动前的水平。此外,SC可能受交感神经的调节,可能是运动期间IOP变化的重要诱发因素。
原文出处:
Li, M., et al., Postexercise Recovery of Schlemm's Canal and Intraocular Pressure in Healthy Individuals: An Observational Study Using Swept-Source Optical Coherence Tomography. J Ophthalmol, 2018. 2018: p. 8513760.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#健康人#
38
#眼压#
33
#THA#
26
学习了
69