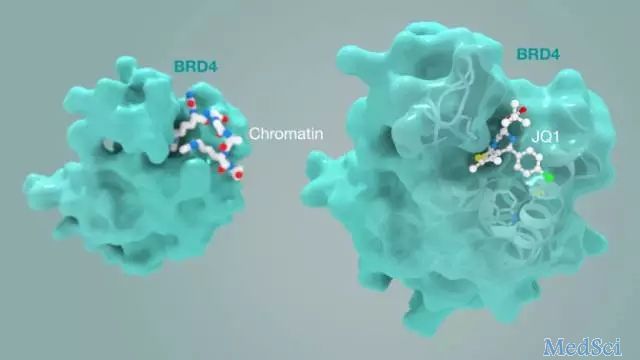
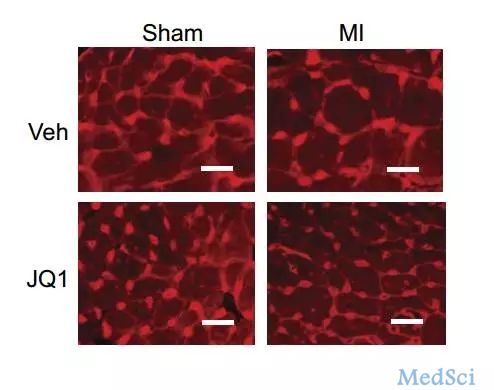
Sci Trans Med:科学家发现抑癌小分子竟能扭转心衰!
2017-05-28 朱爽爽 奇点网
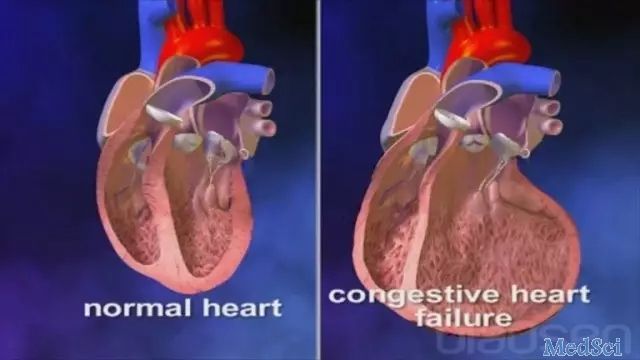
在许多国家,心血管疾病已经成为死亡率最高的“第一大杀手”了,而心血管疾病“走入末路”时导致的就是心力衰竭,尽管一些治疗心衰的药物已经被广泛使用,但是心力衰竭的患者在初次诊断后5年内的死亡率仍然高达40%(1)!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#小分子#
29
#TRA#
21
#科学家发现#
27
#抑癌#
34
#Med#
20
文章不错,拜读了
63
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
56
学习
75