NEC的人工智能(AI)帮助医生确定结直肠病灶有无癌变
2021-07-15 国际文传 网络
NEC Corporation (NEC; TOKYO: 6701)今天宣布一项人工智能技术取得进展,该技术可帮助医生确定结直肠病灶是否属于癌变。NEC开发了一项名为“Cx20&
NEC Corporation (NEC; TOKYO: 6701)今天宣布一项人工智能技术取得进展,该技术可帮助医生确定结直肠病灶是否属于癌变。NEC开发了一项名为“Cx20”的新技术,同时寻求早期检出结直肠病灶的辅助手段。Cx20已达到欧洲安全、健康和环保标准CE标志的要求,并将整合到医疗器械AI诊断支持软件“WISE VISION® Endoscopy”(*1)中,预计将于今年下半年开始在欧洲销售。
该软件可与现有内镜设备连接并相互作用,并根据内镜检查过程中捕获的图像自动通知用户病灶有无癌变可能。其次,该软件可作为一种额外的工具,快速用于辅助内镜医师鉴别病灶并减轻患者负担。
结直肠癌起源于癌前病灶(结直肠癌性息肉),通过在内镜检查过程中检出和摘除早期病灶,有可能抑制其进展。然而,内镜医师在内镜检查时有时难以通过视检鉴别病灶有无癌变,导致不必要的活检和非癌变病灶的摘除,从而给患者造成更多压力和不适。结直肠癌据说是欧洲地区第二大癌症(*2),而在欧洲率先上市的最新版WISE VISION® Endoscopy有望帮助医生解决这一挑战性问题。
为了提高识别结直肠病灶有无癌变可能的机率,并由此帮助内镜医师做出决策,NEC开发了一项新技术,利用AI学习能力整合内镜图像信息与专科医生发现的数据。具体而言,该技术会分析内镜器械拍摄的病灶静止图像,如果AI确定某个结直肠病灶可能属于癌变,则会显示“可能性大”的通知消息。
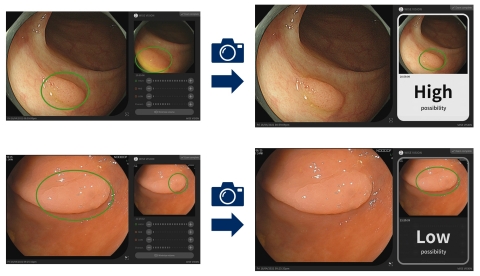
Cx20功能支持病变识别:在检查过程中,通过内镜器械拍摄的视频自动检测疑似病灶。然后医生提取静止图像(左),快速分析并显示结果(右)(图示:美国商业资讯)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#NEC#
40
👍
60
#结直肠#
29
#癌变#
58
谢谢 学习了
93