导语:Avacopan对ANCA相关性血管炎的作用
抗中性粒细胞胞浆抗体(ANCA)相关血管炎的患者容易发生危及生命的并发症,包括进行性局灶性坏死性肾小球肾炎引起的肾功能损害。ANCA相关血管炎也可能由于器官损害,药物(包括长期使用糖皮质激素)毒性等而导致生活质量下降。
在ANCA相关血管炎发病机理中,替代补体途径激活导致末端C5a的产生是重要原因之一。Avacopan是一种口服的小分子C5a受体拮抗剂,可选择性地通过C5a受体(C5aR,也称为CD88)阻断C5a的作用,包括阻断中性粒细胞的化学引诱和激活。 在与ANCA相关的血管炎的小鼠模型中,avacopan预防了由抗髓过氧化物酶抗体诱导的肾小球肾炎的发展。Avacopan在2期试验中显示出对血管炎的作用。研究人员由此进行了一项3期随机试验(ADVOCATE),该试验比较了avacopan与逐渐减少的泼尼松在同时接受免疫抑制药物治疗的ANCA相关血管炎患者身上的作用。

在这项随机对照试验中,研究人员以1:1的比例分配患有ANCA相关血管炎的患者,以每日两次30 mg的剂量口服Avacopan或按逐渐减量的方案口服泼尼松。所有患者均接受环磷酰胺(随后是硫唑嘌呤治疗)或利妥昔单抗治疗。第一个主要终点是缓解,定义为第26周的伯明翰血管炎活性评分(BVAS)为0(等级从0到63,评分越高表示疾病活动越多),并且在之前的4周中未使用糖皮质激素。 第二个主要终点是持续缓解,定义为在第26周和第52周均缓解。两个终点均经过了非劣性(差20个百分点)和优越性测试。
共有331例患者接受了随机分组。166人被分配至Avacopan组,165人被分配至泼尼松组。两组在基线时的平均BVAS为16。在第26周时(第一个主要终点),Avacopan组的166名患者中有120名患者(72.3%)缓解,泼尼松组的164名患者中有115名患者(70.1%)缓解(估计的普遍差异为3.4个百分点;置信区间为95%[ CI],-6.0至12.8;非劣效性P <0.001;优越性P = 0.24)。在第52周时(第二个主要终点),Avacopan组的166位患者中有109位(65.7%)持续缓解,泼尼松组则有90位(54.9%)患者观察到持续缓解(估计的共同差异为12.5个百分点; CI为95%,2.6至22.3;非劣质性,P <0.001;优越性,P = 0.007)。严重的不良事件(不包括恶化的血管炎)发生率在Avacopan组为37.3%,泼尼松组为39.0%。
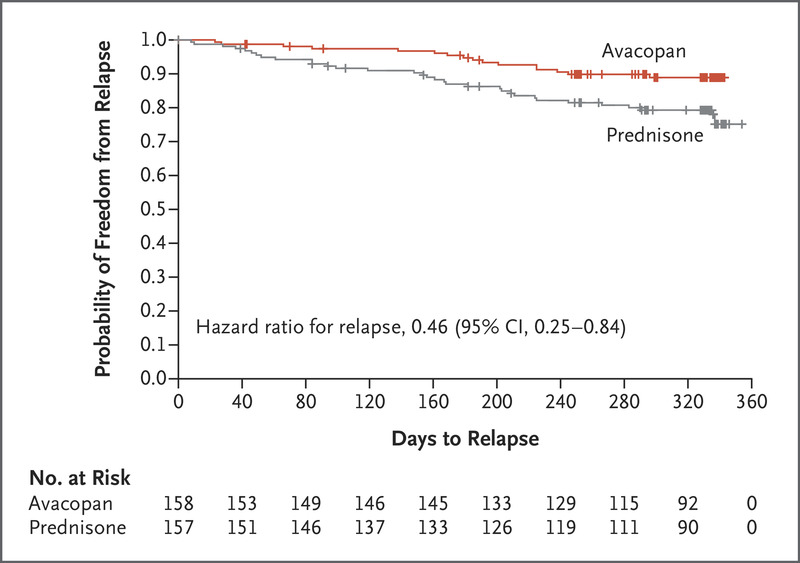
实验结论表明 ,在这项涉及ANCA相关血管炎患者的试验中,Avacopan在26周时的缓解率不低于泼尼松,但在52周时的持续缓解方面优于泼尼松。所有患者均接受了环磷酰胺或利妥昔单抗治疗。 该试验未讨论avacopan超过52周的安全性和临床疗效。
原文链接:https://www.nejm.org/doi/full/10.1056/NEJMoa2023386?query=featured_home
Avacopan for the Treatment of ANCA-Associated Vasculitis
David R.W. Jayne, M.D., Peter A. Merkel, M.D., M.P.H. February 18, 2021 N Engl J Med 2021; 384:599-609 DOI: 10.1056/NEJMoa2023386
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#相关性#
47
#血管炎#
43
#ANCA#
42
#avacopan#
37
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
63