Cell Transplant:间充质基质细胞对骨折的临床改善
2022-09-06 医路坦克 MedSci原创
骨折是指由于巨大的外力(坠落、车祸、撞击等)造成的完整骨骼的断裂,目前还没有推荐用于加速骨折愈合进展的理想治疗方法,本研究的目的是对骨髓间充质干细胞治疗骨修复的动物和临床研究进行系统综述
骨折是指由于巨大的外力(坠落、车祸、撞击等)造成的完整骨骼的断裂。而且大多数发生在儿童和老年人身上。目前还没有推荐用于加速骨折愈合进展的理想治疗方法。因此,需要新的治疗靶点来治疗骨折,缩短骨愈合时间。
间充质基质细胞(MSCs)是具有自我更新能力的多潜能基质细胞,具有分化为肌肉细胞、软骨细胞、脂肪细胞、成骨细胞和其他细胞的潜能。MSCs可以从各种来源分离出来,如脂肪组织、骨髓、肌腱、脐带血、胎儿。此外,MSCs也很容易培养和扩增,并且具有免疫学惰性。MSCs最近被报道用于治疗烧伤、心肌梗死、溃疡性结肠炎、系统性硬化症和其他疾病。作为创伤后诱导组织再生的储备力量,MSCs因其在骨折愈合和骨再生方面的治疗潜力而被广泛研究。最近有报道称,骨髓间充质干细胞可以促进骨愈合。
在这方面,最近的一些动物研究和临床试验已经报道了骨髓间充质干细胞在治疗骨折愈合方面的好处。然而,骨髓间充质干细胞在骨修复或强化方面的临床效果尚未确定。此外,对于哪种细胞来源、细胞类型、剂量和给药方法对患者最有利,几乎没有达成共识。因此,本研究的目的是对骨髓间充质干细胞治疗骨修复的动物和临床研究进行系统综述。
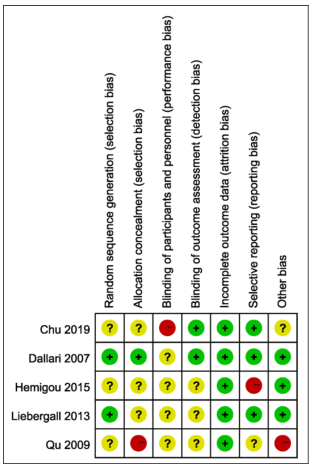
纳入研究的质量评价,使用Cochrane Rob工具对纳入的临床试验进行质量评估
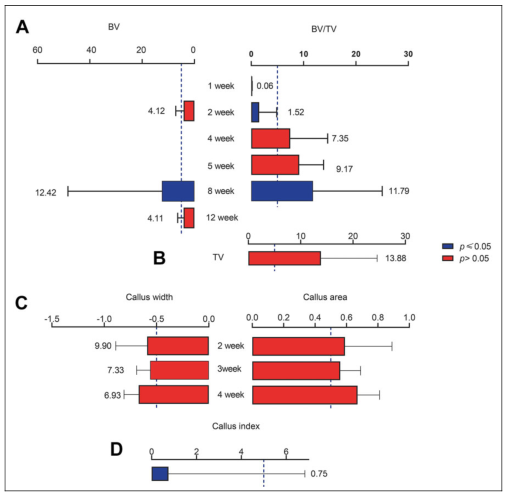
对BV、BV/TV、TV、骨痂宽度、骨痂面积和骨痂指数进行亚组分析。(A)第2、8、12周BV亚组分析,第1、2、4、5、8、12周BV/TV亚组分析。(B)电视的综合分析。(C)第2、3、4周时骨痂宽度和骨痂面积的亚组分析。(D)愈伤组织指数的综合分析。所有分析均采用随机或固定效应模型,可信区间为95%。BV,骨体积;TV,组织体积
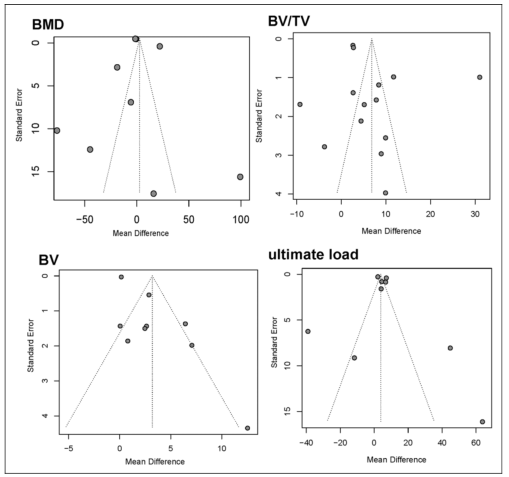
主要和次要结果的漏斗图。生成了BMD、BV、BV/TV和极限负荷的漏斗图
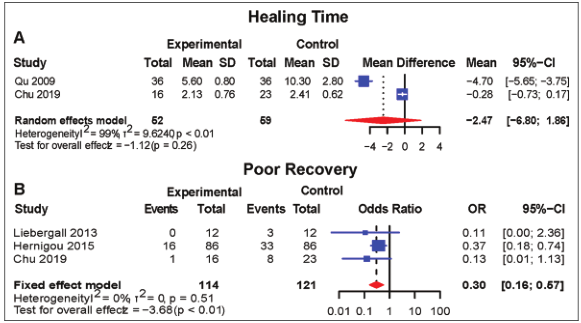
临床转归为愈合时间长、恢复差。(A)愈合时间和(B)恢复不良比率的合并分析
通过输入搜索词和检索截至2021年3月发表的研究,搜索了多个数据库,包括PubMed、EMBASE、Web of Science和Cochrane Library,以确定符合条件的研究。计算平均差值(MD)和95%可信区间(95%CI)来分析Meta分析中的主要结果。数据分析采用Engauge Digiizer10.8和R Software。在31篇文章中,26篇是临床前研究(913篇),5篇是临床试验(335篇)。MSCs治疗显著促进了骨再生的进展[(骨体积与组织体积之比(MD7.35,p<0.01)],尽管对骨痂指数、骨强度、功到失效和僵硬没有显著影响。在临床上,MSC组康复不良的发生率显著降低(优势比(OR)0.30,p<0.01),但愈合时间没有明显缩短(MD 2.47,p.0.26)。
综上所述,我们的数据表明,骨折患者受益于骨髓间充质干细胞的治疗,并且骨髓间充质干细胞是一种潜在的骨再生剂。尽管有这些令人满意的结果,但需要更大规模的随机临床试验(RCT)来证实这些发现。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#CEL#
74
#Cell#
88
#基质#
48
#plant#
46
#TRA#
40
#Transplant#
56
学习了
34