Blood:NADPH氧化酶通过限制LTB4来调控真菌细胞壁诱导的肺中性粒细胞浸润
2020-01-19 QQY MedSci原创
中心点:中性粒细胞NADPH氧化酶通过控制钙离子流入来限制LTB4的生成。LTB4是促进CGD小鼠对真菌细胞壁反应的中性粒细胞炎症的主要驱动因素。摘要:白细胞烟酰胺腺嘌呤二核苷酸磷酸(NADPH)氧化酶在宿主防御和免疫调节中起关键作用。NADPH氧化酶的遗传缺陷可导致慢性肉芽肿病(CGD),其特征是反复发生的细菌和真菌感染以及异常的炎症。在CGD中,由真菌细胞壁引起的超级炎症的关键驱动因素仍未完全
中性粒细胞NADPH氧化酶通过控制钙离子流入来限制LTB4的生成。
LTB4是促进CGD小鼠对真菌细胞壁反应的中性粒细胞炎症的主要驱动因素。
摘要:
白细胞烟酰胺腺嘌呤二核苷酸磷酸(NADPH)氧化酶在宿主防御和免疫调节中起关键作用。NADPH氧化酶的遗传缺陷可导致慢性肉芽肿病(CGD),其特征是反复发生的细菌和真菌感染以及异常的炎症。在CGD中,由真菌细胞壁引起的超级炎症的关键驱动因素仍未完全明确。
近期,研究人员发现,与野生型(WT)中性粒细胞相比,CGD (无CYBB)中性粒细胞经酵母聚糖或免疫复合物激活后,在体外可产生更多的白三烯B4 (LTB4)。这与CGD中性粒细胞钙内流增加有关;而在WT中性粒细胞中,钙内流受NADPH氧化酶电活性抑制。
与LTB4受体BLT1的旁分泌交叉作用进一步放大了CGD中性粒细胞生成的LTB4增多。
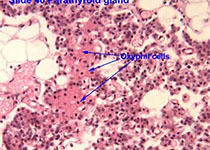
在体外,与同样依赖LTB4-和BLT1的WT相比,在酵母聚糖存在的情况下,CGD中性粒细胞可形成更多更大的团簇。与WT小鼠相比,在酵母聚糖诱导的肺部炎症中,CGD小鼠局灶中性粒细胞浸润增加,并伴有LTB4水平升高。
酵母聚糖刺激后抑制LTB4合成或拮抗BLT1受体可将CGD小鼠肺部的中性粒细胞的募集降低至WT水平。因此,LTB4是CGD小鼠对真菌细胞壁早期反应中嗜中性粒细胞肺炎症的主要驱动因素,可能是因为涉及嗜中性粒细胞产生LTB4的前馈回路失调造成的。
本研究提示中性粒细胞LTB4的生成是NADPH氧化酶调控的一个靶点,或可用来减轻CGD的过度炎症。
原始出处:
Zhimin Song, et al.NADPH oxidase controls pulmonary neutrophil infiltration in the response to fungal cell walls by limiting LTB4.JANUARY 17, 2020
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#中性粒细胞浸润#
30
#LTB4#
25
#中性粒细胞#
27
#真菌#
24
#NAD#
32