Biosci Rep:研究揭示RNA DANCR在人滑膜间充质干细胞软骨形成分化的机制
2017-09-24 MedSci MedSci原创
研究已经发现miRNA可通过调节多种信号通路来调节细胞分化。长链非编码RNA(lnc RNA)DANCR被认为是人类滑膜间充质干细胞(SMSC)的软骨形成的关键,然而,其潜在的分子机制目前尚未清楚。本研究中个,研究人员发现,SMSCs中DANCR的miRNA表达谱过表达确定miR-1305明显下调,而miR-1305是DANCR的下游靶标。值得注意的是,miR-1305过表达逆转了DANCR诱导的
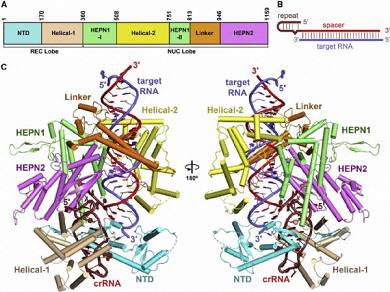
研究已经发现miRNA可通过调节多种信号通路来调节细胞分化。长链非编码RNA(lnc RNA)DANCR被认为是人类滑膜间充质干细胞(SMSC)的软骨形成的关键,然而,其潜在的分子机制目前尚未清楚。
本研究中个,研究人员发现,SMSCs中DANCR的miRNA表达谱过表达确定miR-1305明显下调,而miR-1305是DANCR的下游靶标。值得注意的是,miR-1305过表达逆转了DANCR诱导的SMSCs细胞增殖和软骨形成分化,表明miR-1305拮抗了DANCR的功能。
总之,该研究结果表明miR-1305-Smad4轴作为lncRNA DANCR的主要下游单位,促进SMSCs中软骨的形成。
原始出处:
Lei Zhang, Xiangyi Sun, et al., Long noncoding RNA DANCR regulates miR-1305-Smad 4 axis to promote chondrogenic differentiation of human synovium-derived mesenchymal stem cells. Biosci Rep. 2017 Aug 31; 37(4): BSR20170347. Prepublished online 2017 Jul 3. Published online 2017 Jul 21. doi: 10.1042/BSR20170347
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#DANCR#
43
#Bio#
29
#间充质干细#
32
学习
58
谢谢分享.学习了!
58
谢谢分享.感觉收获很大!
57