Clin cancer research:多参数MR-RET成像可预测复发性高级别神经胶质瘤对GDC-0084治疗的反应性
2020-07-03 QQY MedSci原创
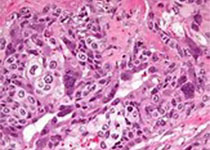
GDC-0084是一种 PI3K/AKT/mTOR信号通路小分子抑制剂,为治疗多形性成胶质细胞瘤 (GBM) 而开发,通过影像学检查是否可评估GBM患者对GDC-0084治疗的反应性?
方法:对GDC-0084 (NCT01547546)的I期试验的47位复发性恶性神经胶质瘤患者进行多参数高级MR-PET成像,评估患者采用GDC-0084治疗的反应。
结果:测得的最大浓度(Cmax)与肿瘤增强信号体积减少(P =0.0287)和分数各向异性增加有关 (FA; P = 0.0418)。治疗后肿瘤体积、18F-FDG 摄取、Ktrans和相对脑血液量(rCBV)均与Cmax相关。18F-FDG PET摄取、表观扩散系数(ADC)、FA、Ktrans、vp和rCBV变化的线性组合能够预估Cmax(R2=0.4113; P<0.0001)和药物暴露 (AUC; R2=0.3481; P<0.0001)。使用此复合多参数MR-PET成像反应生物标记物预测PK,预估Cmax>0.1 μmol/L和AUC>1.25 μmol/L*小时的患者的PFS明显长于低预计浓度和暴露的患者(p值分别是0.0039和0.0296)。
结论:该研究结果表明,通过多参数MR-PET成像创建的针对药物作用机制的代谢和/或生理过程的复合生物标志物,可能有助于更大规模的II-III期试验的疗效评估。
原始出处:
Benjamin M. Ellingson,et al. Multiparametric MR-PET Imaging Predicts Pharmacokinetics and Clinical Response to GDC-0084 in Patients with Recurrent High-Grade Glioma. Clinical Cancer Research. July 01, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#RET#
49
#反应性#
43
#复发性#
46
#神经胶质瘤#
58
#Research#
33