经食管超声心动图诊断主动脉瓣四叶畸形1例
2020-03-18 韩晓明 临床超声医学杂志
患者女,47岁,3年前无明显诱因出现胸闷气短,劳累时加重。体格检查:心界稍扩大,主动脉瓣第1、2听诊区闻及舒张期杂音。心电图检查:窦性心律,心电轴正常,T波改变。胸部X线检查:心尖稍向左侧扩大,心胸比
患者女,47岁,3年前无明显诱因出现胸闷气短,劳累时加重。体格检查:心界稍扩大,主动脉瓣第1、2听诊区闻及舒张期杂音。心电图检查:窦性心律,心电轴正常,T波改变。胸部X线检查:心尖稍向左侧扩大,心胸比为0.56∶1。
超声心动图检查:左室增大,内径55 mm,升主动脉内径正常,室间隔与左室壁厚度正常;左心收缩功能:射血分数56%,短轴缩短率29%,主动脉瓣叶结构不清晰;CDFI:舒张期主动脉瓣可见中量反流信号,缩流颈宽度5 mm,沿二尖瓣前叶走行;连续多普勒:反流峰速440 cm/s,最大压差77 mm Hg(1 mm Hg=0.133 kPa);脉冲多普勒:主动脉瓣上前向最大流速103 cm/s。
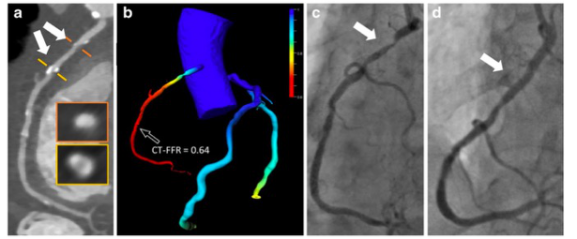
行经食管超声心动图检查:大动脉短轴切面见主动脉窦为四窦,瓣为四瓣,瓣缘增厚,回声增强,呈前后左右排列,左前瓣及右前瓣交界处略粘连,收缩期主动脉瓣开放呈口字形,舒张期关闭呈田字型。开放正常,关闭时可见中央性关闭裂隙,左、右冠状动脉分别起始于左后窦及右前窦(图1,2)。最终诊断为主动脉瓣四叶畸形。

图1 经食管超声心动图示大动脉短轴显示为主动脉瓣关闭状态

图2 经食管超声心动图示主动脉瓣膜呈开放状态
讨论:
主动脉瓣四叶畸形是一种罕见的先天性主动脉瓣病变,其形成机制尚不明确,胚胎学认为很可能是在动脉干分隔早期,因动脉干内膜隆起发育不良导致正常主动脉瓣叶的三个间质原基之一分裂产生第四个瓣叶,主动脉瓣叶出现数目异常及异常瓣叶的增生。
超声心动图是诊断主动脉瓣的主要检查技术,具有高度的敏感性和特异性,但其检查时因声窗观察受限,而经食管超声心动图克服了肺气肿、肥胖、胸廓畸形等因素的影响,可清晰显示主动脉瓣瓣膜结构、数目。因此在常规超声心动图检查发现主动脉瓣瓣叶结构不清,反流原因不明时,应行经食道超声心动图检查以明确诊断,为临床制定治疗方案提供可靠依据。
原始出处:
韩晓明.经食管超声心动图诊断主动脉瓣四叶畸形1例[J].临床超声医学杂志,2019,21(01):20.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#心动图#
39
#主动脉瓣#
30
#畸形#
32
#主动脉#
30
#食管#
35