FDA批准辉瑞EGFR抑制剂达克替尼用于EGFR突变的局部晚期或转移性NSCLC患者的一线治疗
2018-09-28 MedSci MedSci原创
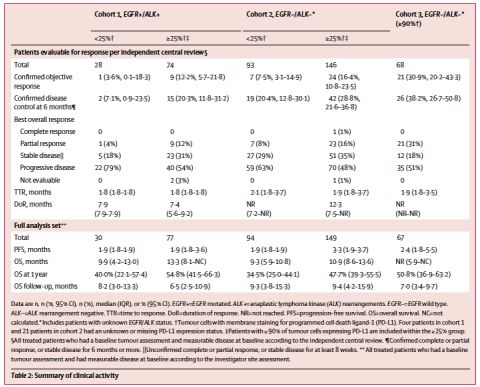
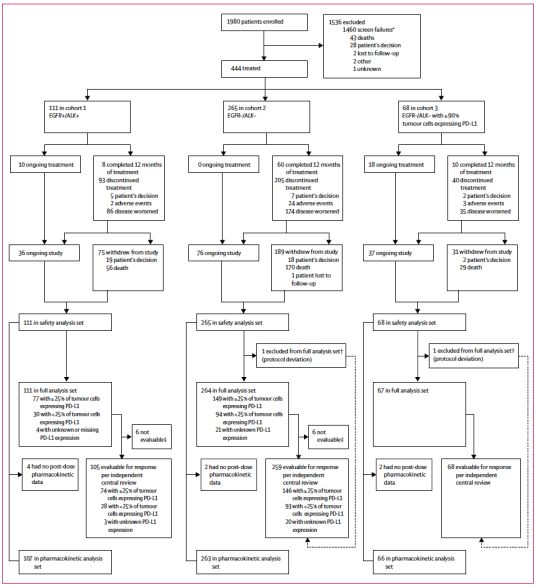
辉瑞的人表皮生长因子受体(EGFR)酪氨酸激酶抑制剂Vizimpro(达克替尼)已在美国被批准用于治疗EGFR突变的局部晚期或转移性非小细胞肺癌(NSCLC)患者的一线治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#局部晚期#
22
#达克替尼#
28
#FDA批准#
31
#转移性NSCLC#
29
#SCLC患者#
19
#抑制剂#
19
#转移性#
27
#局部#
26
#NSCLC患者#
27
#GFR#
28