Lancet Neurol:缺血性卒中前后血压变化不大
2014-03-04 佚名 丁香园
通常大家都会想当然的认为卒中后血压会升高,称之为卒中后高血压。然而,卒中后降压治疗的风险及收益对缺血性卒中和出血性卒中是有差别的,来自英国牛津大学的Urs Fischer等学者对比了这两类卒中急性期及卒中前的血压情况,在线发表在2014年2月28日的Lancet Neurology杂志上。结果显示:缺血性卒中前后血压变化不大,出血性卒中后血压明显升高。【原文下载】 此
通常大家都会想当然的认为卒中后血压会升高,称之为卒中后高血压。然而,卒中后降压治疗的风险及收益对缺血性卒中和出血性卒中是有差别的,来自英国牛津大学的Urs Fischer等学者对比了这两类卒中急性期及卒中前的血压情况,在线发表在2014年2月28日的Lancet Neurology杂志上。结果显示:缺血性卒中前后血压变化不大,出血性卒中后血压明显升高。【原文下载】
此为英国牛津郡基于人口的研究,纳入2002年4月1日至2012年3月31日间的所有卒中患者。对比10年间基础医疗机构记录的缺血性卒中(美国国立卫生研究院卒中量表大于3分)及脑出血患者卒中后急性期血压及患病前血压情况。
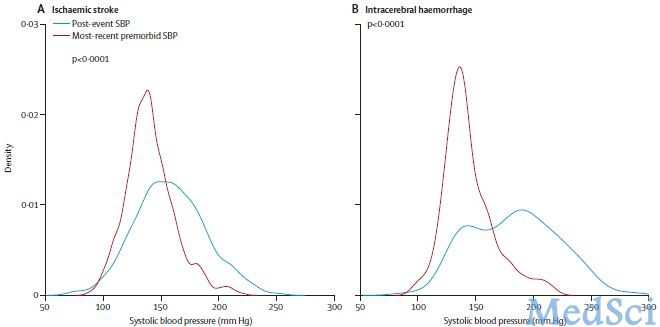
在随机纳入的653例符合纳入标准的患者中,共获得636例患者卒中前及卒中急性期血压临床数据。卒中发生前,共记录13244例次血压,平均在不同场合对每例患者进行平均17次血压测量。缺血性卒中患者卒中急性期的血压明显低于出血性卒中患者,两者平均为158.5 mmHg和189.8 mmHg,相比卒中前轻度增高,平均增高约10.6 mmHg;在卒中后首个24小时内仅有轻度的下降。与缺血性卒中相比,出血性卒中发生后收缩压相比卒中前明显增高,平均增高40.7 mmHg;且在卒中后24小时内下降明显,平均下降41.1 mmHg。出血性卒中发生前几天或几周血压也有明显的升高,然而缺血性卒中却没有此种情况。出血性卒中相比缺血性脑卒中,急性期血压更接近起病前记录的血压最高值。在那些起病90分钟内就诊的脑出血患者,起病3小时内的最高收缩压相比卒中前的最高血压平均高出50 mmHg,然而对于缺血性脑卒中患者,起病后的最高血压却低于卒中前的最高血压,约低5.2 mmHg。
缺血性卒中与出血性卒中发生前平均血压及卒中后首次血压对比
该研究提示脑出血后收缩压相比发病前有明显的升高,而缺血性卒中急性期收缩压却更接近于患者起病前的一贯血压水平。该研究结果在一定程度上解释了为什么卒中后快速降压治疗在风险及获益方面会有不同。
原始出处:
Urs Fischer MD a †, Marie Therese Cooney PhD a †, Linda M Bull RN a, Louise E Silver DPhil a, Prof John Chalmers MD b, Prof Craig S Anderson MD b, Ziyah Mehta DPhil a, Prof Peter M Rothwell FMedSci.Acute post-stroke blood pressure relative to premorbid levels in intracerebral haemorrhage versus major ischaemic stroke: a population-based study.The Lancet Neurology, 28 February 2014 doi:10.1016/S1474-4422(14)70031-6【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
34
#血压变化#
27
#Neurol#
27
#缺血性#
37
#缺血性卒#
32