Circulation:两机构联合推出儿科肺动脉高压临床治疗指南
2015-11-04 姜英浩 MedSci原创
2015年11月3日,美国心脏学会(The American Heart Association)与美国胸科学会( American Thoracic Society)在Circulation杂志上联合发布了第一版的评估和治疗儿科肺动脉高压( pulmonary hypertension , PH)的临床实践指南。两机构联合推出这份实践指南的目的基于在临床上,新生儿、幼儿的PH发病原因与治疗方式均
2015年11月3日,美国心脏学会(The American Heart Association)与美国胸科学会( American Thoracic Society)在Circulation杂志上联合发布了第一版的评估和治疗儿科肺动脉高压( pulmonary hypertension , PH)的临床实践指南。
两机构联合推出这份实践指南的目的基于在临床上,新生儿、幼儿的PH发病原因与治疗方式均与成人有较大不同。当前关于成人PH的文献十分充分,并且已有若干相关的治疗指南出台,然而关于儿童PH却缺乏足够的研究。“对于儿童PH的发病原因、机制以及治疗手段,目前我们几乎一无所知。”该指南的编写委员会联合主席之一,美国科罗拉多大学与儿童医院的小儿胸腔科教授 Steven H. Abman表示道,“值得注意的是,尽管既往的指南为治疗儿童肺动脉高压建立了一定的基础,目前我们仍然需要大量的详细的数据和研究以提高未来治疗的效果。”
本指南由27位小儿胸腔科、小儿与成人心脏病学、小儿重症监护科、新生儿科以及转化医学界的的临床医师和研究专家合作,在参考了600余篇文献后完成。但是由于关于儿科PH的高质量临床数据缺乏,本篇指南更大程度地依赖专家的个人经验和意见,并且在诊断和治疗指南中主要描述为“一般情况下可接受的方法”,更多细致和精确的指导仍然需要未来的研究结果来提供信息。
儿科PH被定义为在出生后几个月内,发生的静息肺动脉压高于25 mmHg的症状,通常与心脏、肺部或系统性疾病相关。先天性PH,是一种肺部血管病变,通常在确定左心、肺实质、心脏瓣膜、血栓栓塞等并未发生疾病后,得到了排除诊断确诊。
本指南强调了被怀疑患有PH的儿童应当在特殊的儿科专科治疗中心接受综合性的全面治疗和管理。本指南的另一位联合主席,英国女王大学医学院院长Stephen L. Archer教授表示:“当孩子被诊断患有PH时,家长通常会感到很无助。其实他们应该及时寻找到那些经常接诊这样患者的医师和医院,他们能够用最新的诊断、最新的药物、设备和手术手段对孩子给予治疗。事实上,患有PH的儿童会在一生中都伴随着健康问题,或在很小时候就死亡,尤其是在他们未接受到合适的诊断和治疗的情况下。但是,如果他们能在PH特诊中心接受相应的诊断和治疗,其大部分患儿的预后是相当不错的。”
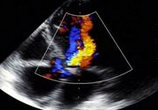
对于PH疾病的恰当分级是决定治疗成功的关键的第一步。本指南提供了大量诊断和观测PH的方法,包括了影像学研究、心电图、心导管检查术、脑促尿钠排泄肽及其他实验学检查、6分钟行走距离(针对适当的年龄范围)、睡眠研究以及基因检测等。它能针对性解决新生儿持续性PH,从先天性膈疝、支气管肺发育异常及其他肺部疾病、房间隔缺损和动脉导管未闭等心脏疾病、溶血性血红蛋白病及肝、肾、代谢等系统性疾病发展形成的PH,以及先天性PH和高空性肺水肿相关的PH等。
关于门诊护理的提升方面,该指南建议接诊患PH的儿童时给予流感、肺炎以及呼吸道合胞体病毒疫苗接种,并对面部出现青紫的或置有中央静脉导管的患儿给予抗体以预防亚急性细菌性心内膜炎。整个成长环境都处在严密的观察下,对任何感染和呼吸系统疾病都应及时发现和处理。对患儿的任何手术治疗都应在PH的专家在场的情况下,经过严谨地规划方能实施。
本指南中还有一章详细地讲述了对儿童PH的药物治疗,包括了洋地黄、利尿剂、长期抗凝药物、氧疗、钙离子通道阻断剂、磷酸二酯酶5抑制剂、内皮素受体拮抗剂、静脉或皮下环前列腺素治疗等,以及逐渐由非肠道至口服和吸入疗法的转变。
此外,本指南还提到了体育锻炼、旅行受限、对患儿父母的避孕咨询等。指南在最后建议,鉴于儿童PH会对整个家庭,包括患者、父母、亲属以及其他护理人员都会造成社会和心理压力,因此需要得到及时和足够的社会和医学支持。
原始出处:
Robert W. Neumar, et al. 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015.11.3
MARY ANN MOON. Family Practice News Digital Network. 2015.11.3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉高压#
44
#治疗指南#
42
好!
111
#临床治疗#
42
好文
91