Mayo Clin Proc:成人慢性阻塞性肺疾病心肌梗死后心脏选择性与非选择性β受体阻滞剂的比较
2022-03-14 从医路漫漫 MedSci原创
慢性阻塞性肺疾病(COPD)的特点是进行性气流受限,并与肺部的异常炎症反应有关。此外,COPD是一种高度全身性炎症状态,可能导致动脉粥样硬化、斑块破裂和血栓形成。

背景:慢性阻塞性肺疾病(COPD)的特点是进行性气流受限,并与肺部的异常炎症反应有关。此外,COPD是一种高度全身性炎症状态,可能导致动脉粥样硬化、斑块破裂和血栓形成。观察性研究报告COPD导致冠状动脉疾病、心绞痛、心肌梗死(MI)和中风,也导致MI后预后不良。因此,心血管事件在COPD患者中并不少见,以及如何最好地提高MI后COPD患者的存活率。
一些临床试验已经报道了β-受体阻滞剂可以减少MI患者的全因死亡和不良心脏事件的发生率。然而,在一些观察性研究中,β-受体阻滞剂被报道会诱发支气管痉挛和导致肺功能的急性恶化,因此大多数临床医生没有给患有COPD的MI患者开β-受体阻滞剂。实际上,这意味着COPD患者在住院期间和在MI之后往往得不到足够的治疗。然而,一些研究报告了心脏选择性β-受体阻滞剂。一些研究报道β受体阻滞剂对各种原因的死亡率有保护作用,并能改善COPD患者心肌梗死后的短期存活率。然而,缺乏大规模研究,目前尚不清楚心脏选择性或非选择性β受体阻滞剂是否能提高COPD心肌梗死患者的整体长期生存率。因此,我们设计了这项研究,利用来自台湾全国数据库的数据,研究心脏选择性或非选择性β-受体阻滞剂对首次心肌梗死后慢性阻塞性肺疾病患者全因死亡率和不良事件的影响。
目的:探讨β受体阻滞剂在慢性阻塞性肺疾病(COPD)合并心肌梗死(MI)患者中的疗效和安全性,以解决慢性阻塞性肺疾病(COPD)合并心肌梗死(MI)患者使用β受体阻滞剂的疑虑。
方法:我们在2001年1月1日至2013年12月31日期间在台湾国家健康保险研究数据库中确定了65,699名首次心肌梗死后服用β-受体阻滞剂的COPD患者。采用治疗概率倒数加权法进行比较。主要结果是全因死亡率;次要结果是心力衰竭住院、主要不良心脑血管事件(MACCE)和主要不良肺部事件(MAPE)。
结果:共有14789名服用β-受体阻滞剂的患者入选,其中7247名(49.0%)使用心脏选择性β-受体阻滞剂,7542名(51.0%)使用非选择性β-受体阻滞剂。心脏选择组的死亡率(危险比,0.93;95%CI,0.89~0.96)、MACCE发生率(HR,0.96;95%CI,0.93~0.998)、心力衰竭住院发生率(次分布HR,0.84;95%CI,0.78~0.91)和MAPE发生率(HR,0.94;95%CI,0.90~0.98)较低。在比索洛尔处方和卡维地洛处方之间的亚组分析中也发现了类似的结果。
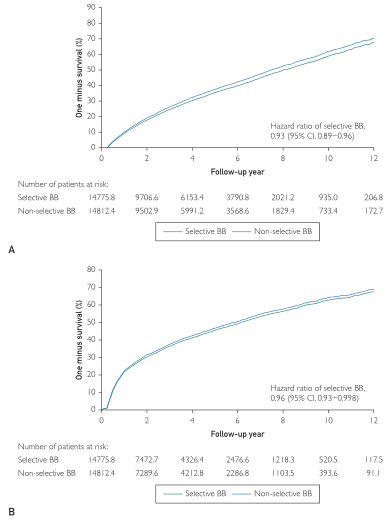
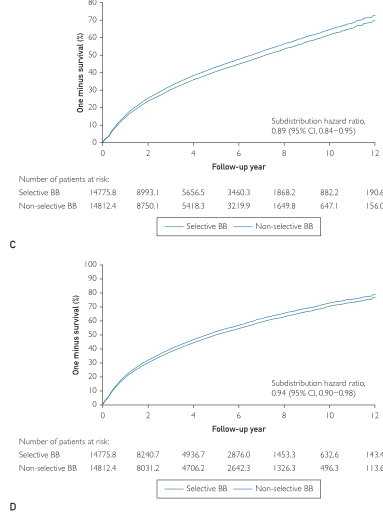
图1.Kaplan-Meier 1减去生存曲线图显示,与心肌梗死后服用非选择性b-受体阻滞剂的患者相比,服用心脏选择性b-受体阻滞剂(BB)的慢性阻塞性肺病患者的全因死亡率(A)、主要不良心脑血管事件(B)、心力衰竭住院(C)和主要不良肺部事件(D)的发生率较低,这与治疗权重队列中使用非选择性b-受体阻滞剂的概率相反。

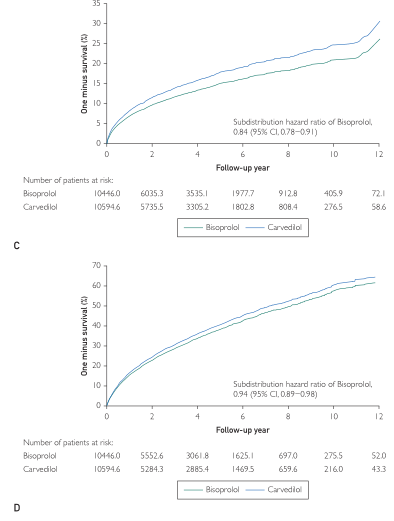
图2.Kaplan-Meier 1减去生存曲线图显示,在治疗权重队列中,与心肌梗死后服用卡维地洛的患者相比,服用比索洛尔的慢性阻塞性肺病患者的全因死亡率(A)、主要不良心脑血管事件(B)、心力衰竭住院(C)和主要不良肺部事件(D)的发生率较低。

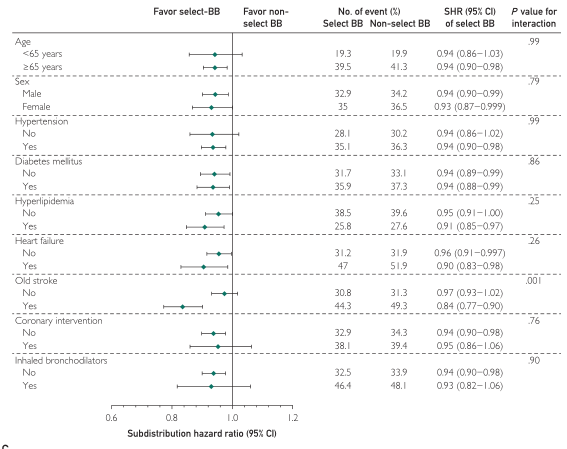
图3.接受选择性与非选择性b-受体阻滞剂(BB)治疗加权队列的心肌梗死和慢性阻塞性肺病患者的全因死亡率(A)、主要不良心脑血管事件(B)和主要不良肺部事件(C)的亚组分析。
结论:与非选择性β受体阻滞剂相比,使用心脏选择性β受体阻滞剂的患者全因死亡率、MACCE、心力衰竭住院和MAPE发生率较低。急性心肌梗死后COPD患者住院期间和出院后继续接受心脏选择性β-受体阻滞剂治疗似乎优于非选择性β-受体阻滞剂治疗。
原文出处:Chung CM, Lin MS, Chang ST,et al.Cardioselective Versus Nonselective β-Blockers After Myocardial Infarction in Adults With Chronic Obstructive Pulmonary Disease.Mayo Clin Proc 2022 Feb 05
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
.jpg)










#选择性#
44
#受体阻滞剂#
31
#阻塞#
38
#ROC#
41
#阻滞剂#
40
#β受体阻滞剂#
33
#PRO#
30