严重过敏该如何抢救?收藏这张流程图轻松搞定!
2022-01-07 网络 网络
WAO指南强调了严重过敏反应急救后长期管理的必要性,教育患者严重过敏反应的风险和复发时自我治疗,并为有复发风险的人群开具肾上腺素自动注射器(epinephrine autoinjector,EAI)。
严重过敏反应是急性全身过敏反应最严重的临床表现。全球严重过敏反应的发生率为50~112次/10万人/年,而估计的终生患病率为0.3%~5.1%。儿童严重过敏反应的发生率为1~761/10万人/年。有研究随访1.5~25年发现,26.5%~54.0%的严重过敏反应患者出现复发。估计药物诱发严重过敏反应导致的死亡率为0.05~0.51/百万人/年,食物为0.03~0.32/百万人/年,昆虫毒液为0.09~0.13/百万人/年。
| 认识严重过敏反应
世界过敏组织( World Allergy Organization,WAO)提出最新定义:严重过敏反应是严重的全身性超敏反应,通常发病迅速,可导致死亡,以危及气道、呼吸系统、循环系统为特征,可不合并典型的皮肤表现或循环休克症状。
主要发病机制为IgE介导的I型变态反应,还包括非IgE介导的免疫学或非免疫学机制,常由食物、昆虫叮咬和药物诱发,引起过敏反应的常见药物包括抗生素和非甾体类消炎药。
| 严重过敏反应的治疗
严重过敏反应是一种急症,需迅速识别和处理。对于有既往史患者,急性期治疗包括两步:
1.患者使用紧急方案自救,肌内注射肾上腺素起关键作用;
2.获得医疗救助后,需给予其他干预措施,如症状持续,则必须再次给予肾上腺素治疗。
患者发生严重过敏反应时,应遵循以下步骤:
1)尽可能去除过敏原(例如,停止用药),2)评估气道、呼吸、循环、精神状态和皮肤状况,立即拨打急救电话,3)股四头肌的股外侧肌(大腿中部外侧)肌内注射肾上腺素,4)根据患者的临床表现放置体位。过敏反应时,大多数患者应置于仰卧位,呼吸窘迫者应置于端坐位,孕妇应置于左侧半卧位,意识不清者置于复苏体位。
转送到医疗机构(包括救护车)后对严重过敏反应的处理:
1)对呼吸窘迫患者和接受较大剂量肾上腺素治疗患者提供高流量氧气(最好使用非再呼吸面罩),2)建立静脉通路(成人用14或16号套管),3)循环系统不稳定患者给予静脉输液(晶体液20 mL/kg)。如有指征,可进行持续心脏按压。
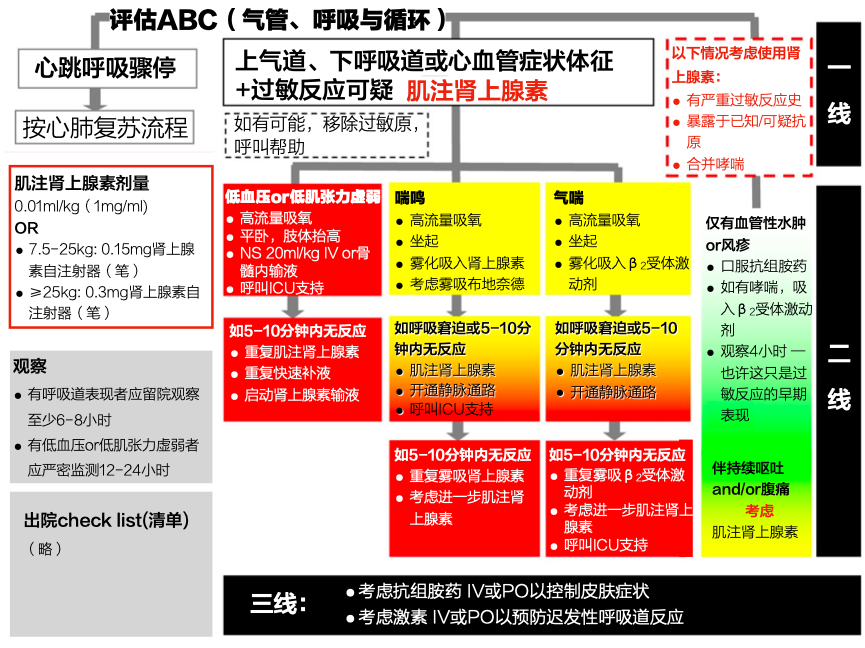
| 严重过敏的抢救流程图
| 严重过敏反应的一线治疗药物
肾上腺素是治疗严重过敏反应的一线药物。
作用机制:肾上腺素通过激动α1受体,收缩周围血管,逆转低血压和黏膜水肿;激动β1受体,增强心脏收缩力,逆转低血压;激动β2受体,逆转支气管收缩并减少炎性递质释放。
剂量:《严重过敏反应急救指南》推荐意见,肾上腺素给药剂量为0.01 mg/kg,14岁及以上患者单次最大剂量不超过0.5 mg,14岁以下患者单次最大剂量不超过0.3mg,浓度为1mg/ml(1:1000),等同于1ml:1mg规格的肾上腺素注射液,肌内注射给药。如症状不缓解,间隔5~15min重复给药一次。
肌内注射肾上腺素通常耐受性良好。而静脉注射肾上腺素可造成致命的心律失常,因此,不推荐静脉注射肾上腺素用于严重过敏反应的初始治疗,如使用,最好通过输液泵。
尽管国际指南建议在所有情况下将肌内注射肾上腺素用于过敏反应一线治疗,但最新过敏反应相关心脏骤停的高级生命支持指南指出,如果心脏骤停即将发生或已经发生,则需要静脉推注肾上腺素。
| 严重过敏反应的其他药物
二线治疗药物包括β2受体激动剂、糖皮质激素和抗组胺药。
-
对伴有支气管狭窄的严重过敏反应,可给予吸入短效 β2受体激动剂,若症状持续存在,吸入或雾化吸入支气管扩张剂不能替代重复肌内注射肾上腺素。
-
H1受体拮抗剂对严重过敏反应的作用有限,主要用于缓解皮肤症状,目前仅可静脉给药(如氯苯那敏,苯海拉明,氯马斯汀),但快速静脉给药(如氯苯那敏)会引起低血压。且使用二线药物可能会延迟一线药物肾上腺素的使用。仍需高质量随机对照研究探索抗组胺药物在严重过敏反应中的作用。
-
糖皮质激素常用于治疗严重过敏反应,以预防长期症状。然而,越来越多的证据表明,糖皮质激素对严重过敏反应急性期治疗可能无益,甚至可能有害,但尚无证据表明在过敏反应紧急治疗中使用糖皮质激素会产生不良后果。仍需进一步研究阐明糖皮质激素治疗是否能减少过敏反应中双相反应的发生。
WAO指南强调了严重过敏反应急救后长期管理的必要性,教育患者严重过敏反应的风险和复发时自我治疗,并为有复发风险的人群开具肾上腺素自动注射器(epinephrine autoinjector,EAI)。目前 EAI在国内尚未普及使用,根据国际指南的推荐建议,可考虑在国内推广使用 EAI,以提高过敏反应治疗的及时性。
参考文献:
[1] Vc A , Ija B , Me C , et al. Worldallergy organization anaphylaxis guidance 2020 - ScienceDirect[J]. WorldAllergy Organization Journal, 13( 10).
[2]张紫薇, 骆兵, 葛卫红,等. EAACI与WAO严重过敏反应指南药物急救管理解读及证据分析[J]. 医药导报, 2021, 40(11):6.
[3]骆兵, 张紫薇, 葛卫红,等. EAACI和WAO严重过敏反应指南长期管理解读及证据分析[J]. 医药导报, 2021, 40(11):6.
[4]李晓桐,翟所迪,王强,王育琴,尹佳,陈玉国,陈荣昌,张洪君,杨克虎,李天佐,郑亚安,马青变,刘芳,崔畅,郑航慈.《严重过敏反应急救指南》推荐意见[J].药物不良反应杂志,2019,21(02):85-91.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#抢救#
49
很好的文章,及时
65
学习到了
67
很好
53
总结得很到位
49
学习到了
48