HUMAN BRAIN MAPPING:pre-SMA与额下回的功能连接增强与强迫症的运动反应抑制能力相关
2022-01-23 影像小生 MedSci原创
该研究强调了前SMA和IFG之间功能连接的改变对OCD运动反应抑制病理生理学的重要性。
最近的研究表明,辅助前运动区(pre-SMA)和额下回(IFG)在反应抑制中起重要作用。然而,目前尚未有研究探讨强迫症患者静息态脑网络与反应抑制之间的关系。
Tomohiro Nakao等在HUMAN BRAIN MAPPING杂志发表研究文章,对41名无药物治疗的强迫症患者和49名健康对照(HC)参与者进行了静息态功能磁共振成像扫描,并使用扫描仪外的停止信号任务测量了他们的反应抑制。
该研究探讨了OCD和HC组在与运动反应抑制能力相关的前SMA和IFG功能连接方面的差异。
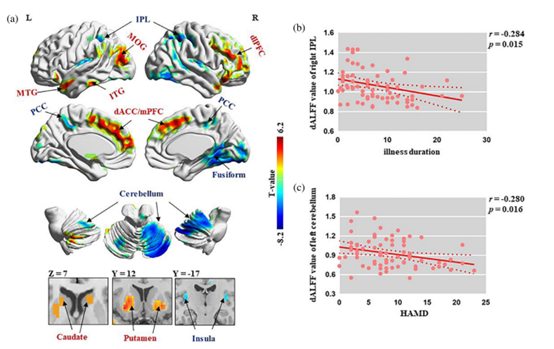
与健康对照组(HC)相比,强迫症(OCD)患者的额下回在内的脑区与右侧pre-SMA的功能连接增加与运动反应抑制更差显著相关。
强迫症患者有较长的停止信号反应时间(SSRT)。
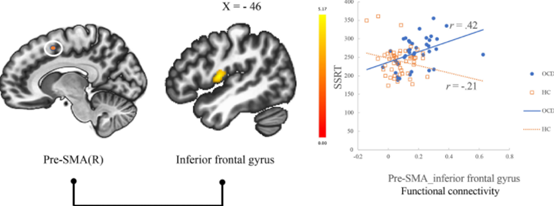
在强迫性障碍(OCD)组中,pre-SMA和IFG间更强的功能连接与反应抑制受损有关。
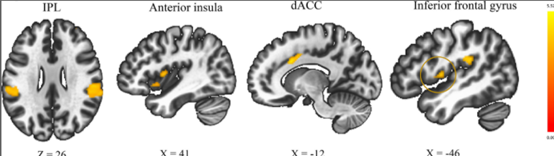
与HC相比,OCD患者的运动反应抑制能力与前SMA和IFG、顶叶下叶、背侧前扣带皮层、岛叶和前前额叶皮层之间的功能连接存在不同的相关性。
进一步的分析表明,与HC相比,OCD在pre-SMA和IFG之间表现出更强的功能连接。此外,这种功能连通性与SSRT得分呈正相关。
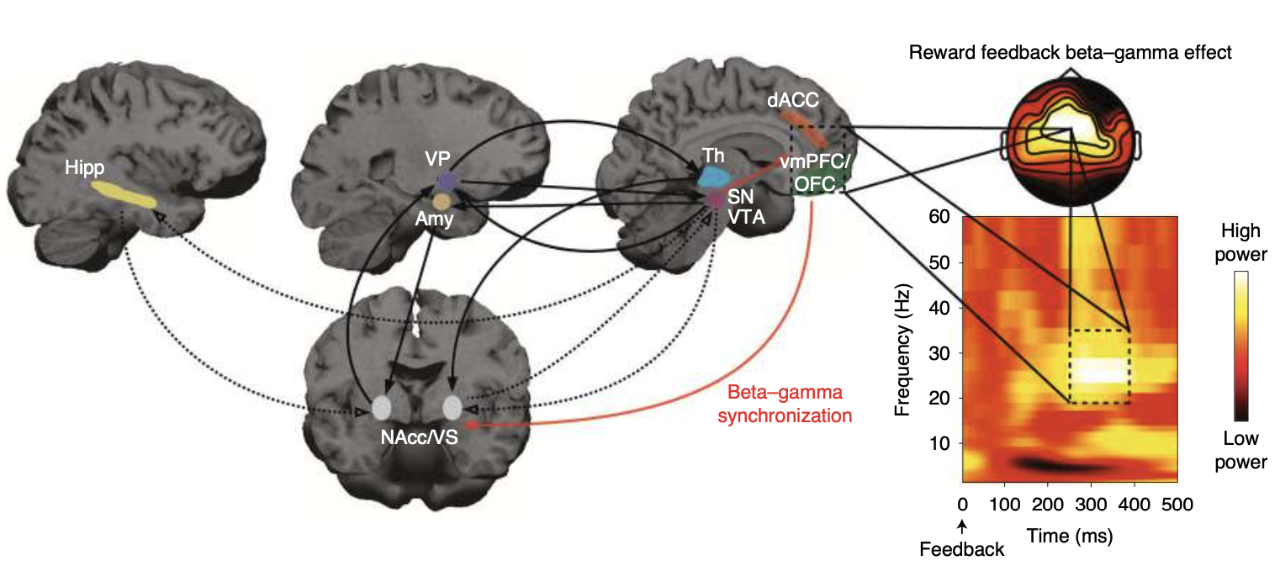
这些结果为属于皮质-纹状体-丘脑-皮质回路和扣带回-盖显著网络的静息状态功能连接的特征提供了额外的见解,这是OCD运动反应抑制受损的基础。特别地强调了前SMA和IFG之间功能连接的改变对OCD运动反应抑制病理生理学的重要性。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











看了一头雾水,还是不知如何去治疗
28
#mapping#
62
#human#
46
学习了,谢谢分享
43
#SMA#
40
#功能连接#
57