JCEM:恶性嗜铬细胞瘤和副神经节瘤预后的相关因素有那些?(大型长期研究)
2017-06-16 MedSci MedSci原创
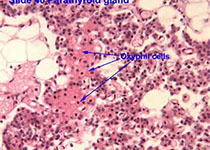
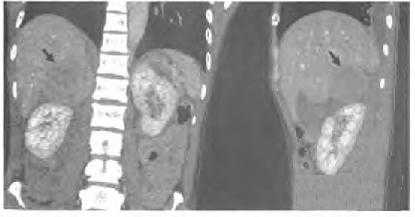
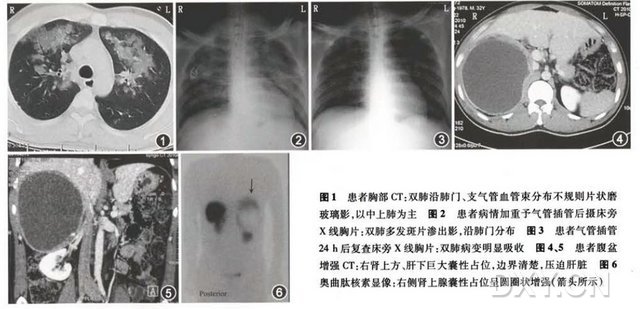
副神经节源肿瘤起源于副交感神经节简称“副节”。副节乃对交感神经干中的神经节相对而言,大多位于交感神经干之侧旁,偶尔亦见于内脏等远离的部位。副节按其主细胞对铬盐的反应有嗜铬性与非嗜铬性之别,故副神经节瘤亦有嗜铬性与非嗜铬性之分。嗜铬性副节瘤以肾上腺髓质为主要代表,由其发生的肿瘤习惯称“嗜铬细胞瘤”(Pheochromocytoma);而非嗜铬性副节发生的肿瘤则往往简称“副节瘤”,文献中也称之为“非嗜
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCE#
32
#JCEM#
33
学习并分享!!!
55
文章很好,拜读了
59
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
54
#相关因素#
22
#细胞瘤#
27
#副神经节瘤#
26
不错的,学习了,谢谢分享!
48
学习了,谢谢分享
51