Heart:对比增强CT评估主动脉瓣狭窄的意义
2021-02-01 MedSci原创 MedSci原创
对比增强CT评估主动脉瓣钙化和非钙化体积的变化与主动脉瓣狭窄程度相关,当纤维化是导致瓣膜阻塞的重要因素时,其评估效能优于非对比CT。
非对比CT主动脉瓣钙化评分忽略了瓣膜纤维化在主动脉瓣狭窄中的意义。近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员旨在使用对比增强CT评估主动脉瓣钙化和非钙化疾病。
这是对164例主动脉瓣狭窄患者(中位年龄为71岁(IQR为66-77岁),男性占78%)进行的事后分析(41例轻度,89例中度,34例重度主动脉瓣狭窄;7%二尖瓣狭窄),他们接受了超声心动图检查和对比增强CT作为影像学检查的一部分。研究人员针对血液放射密度校准的Hounsfield单位阈值对钙化和非钙化(纤维化)的瓣膜组织体积进行定量,并确定瓣环面积。纤维钙化比值用于评估瓣膜纤维化和钙化的相对程度。研究人员将纤维钙化体积(非钙化和钙化体积的总和)与主动脉瓣峰值速度进行比较,并在一个亚组中比较了组织学和瓣膜重量。
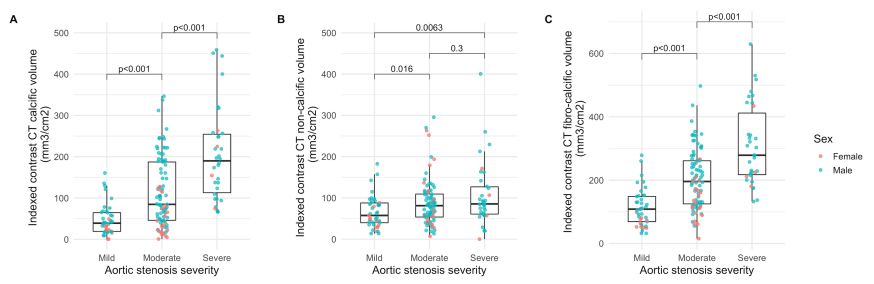
对比增强的CT钙体积与CT钙评分(r=0.80,p<0.001)和主动脉射流峰值速度(r=0.55,p<0.001)相关。纤维钙化比值随主动脉狭窄严重程度的增加而降低(轻度:1.29(0.98-2.38),中度:0.87(1.48-1.72),重度:0.47(0.33-0.78),p<0.001),而纤维化钙化量增加(轻度:109(75-150),中度:191(117-253),重度:274(213-344)mm3/ m2)。纤维钙化体积与离体瓣膜重量相关(r=0.72,p<0.001)。与Agatston评分相比,纤维钙化体积证实与峰值主动脉射流速度具有更好的相关性(分别为r=0.59和r=0.67),特别是在女性患者中(分别为r=0.38和r=0.72)。
由此可见,对比增强CT评估主动脉瓣钙化和非钙化体积的变化与主动脉瓣狭窄程度相关,当纤维化是导致瓣膜阻塞的重要因素时,其评估效能优于非对比CT。
原始出处:
Timothy RG Cartlidge.et al.Contrast-enhanced computed tomography assessment of aortic stenosis.heart.2021.https://heart.bmj.com/content/early/2021/01/28/heartjnl-2020-318556
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#对比增强CT#
39
#增强CT#
38
对比增强CT评估主动脉瓣钙化和非钙化体积的变化与主动脉瓣狭窄程度相关,当纤维化是导致瓣膜阻塞的重要因素时,其评估效能优于非对比CT。
77
#主动脉瓣#
34
#ART#
25
#主动脉#
29
#HEART#
26