Ann Rheum Dis:瑞莎珠单抗治疗对活动性银屑病关节炎的疗效和安全性分析
2021-11-25 MedSci原创 MedSci原创
与安慰剂相比,瑞莎珠单抗治疗可显著改善关键疾病结局,并且对Bio-IR和/或csDMARD-IR的PsA患者具有良好的耐受性。
瑞莎珠单抗是一种白细胞介素23抑制剂,正在研究用于治疗银屑病关节炎(PsA)患者。KEEPsAKE的2期和3期试验探究了瑞莎珠单抗与安慰剂在既往对2种以下生物疗法(Bio-IR)和/或1种以上常规合成疾病缓解抗风湿药反应不足或不耐受的活动性PsA患者(csDMARD-IR)中的疗效和安全性。

近日,风湿病领域顶级期刊Annals of the Rheumatic Diseases上发表了一篇研究文章,该研究报告了PsA患者采用瑞莎珠单抗治疗的第24周的结局。
研究人员将Bio-IR和/或csDMARD-IR的PsA成人随机进行分组,在24周的双盲治疗期间,受试者在第0、第4和第16周接受皮下注射150mg瑞莎珠单抗或安慰剂治疗。该研究的主要终点是第24周美国风湿病学会评分(ACR20)改善≥20%的患者比例,该研究的次要终点评估PsA患者的关键领域和患者报告的结局。
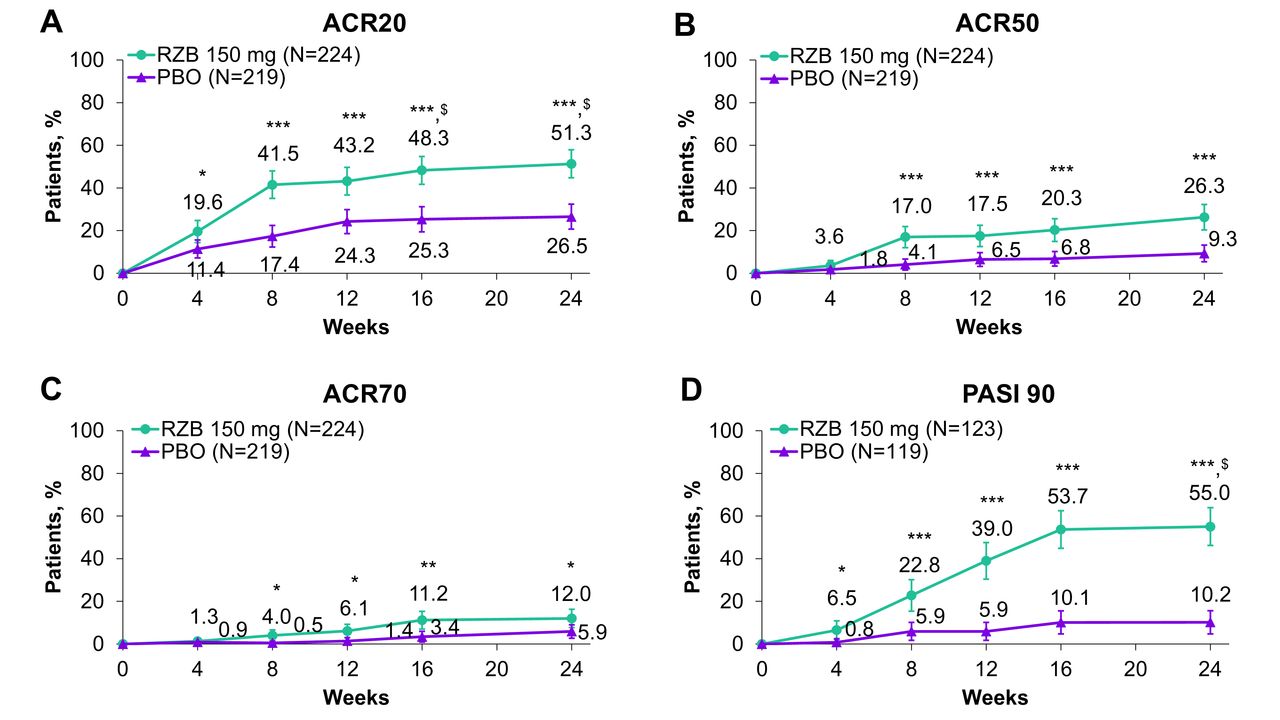
该研究共有444名患者(中位年龄为53岁,范围为23-84岁)被随机分配至接受瑞莎珠单抗(n=224)或安慰剂(n=220)治疗;206名患者(46.5%)为Bio-IR患者。在治疗后的第24周,与安慰剂相比,接受瑞莎珠单抗治疗的患者达到ACR20的主要终点(51.3% vs. 26.5%,p<0.001)和所有次要终点(p<0.05)的比例明显更高。瑞莎珠单抗治疗和安慰剂治疗的患者分别报告了4.0%和5.5%的严重不良事件;据报道,严重感染分别为0.9%和2.3%。
由此可见,与安慰剂相比,瑞莎珠单抗治疗可显著改善关键疾病结局,并且对Bio-IR和/或csDMARD-IR的PsA患者具有良好的耐受性。
原始出处:
Andrew Östör,et al.Efficacy and safety of risankizumab for active psoriatic arthritis: 24-week results from the randomised, double-blind, phase 3 KEEPsAKE 2 trial.Ann Rheum Dis.2021.https://ard.bmj.com/content/early/2021/11/23/annrheumdis-2021-221048
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效和安全性#
42
#活动性#
48
#Dis#
41
#关节炎#
32
#活动性银屑病关节炎#
59